Alcohol use disorder is a significant healthcare issue in Australia. Almost half (43%) of those who received treatment for alcohol and other drug use in 2022-23 considered alcohol their primary concern.
But new research by the University of Western Australia’s School of Population and Global Health found that two medicines indicated and subsidised for the treatment of alcohol use disorder – naltrexone and acamprosate – are largely underutilised.
The research found the use of pharmacotherapies is low compared with the prevalence of alcohol use disorder in Australia.
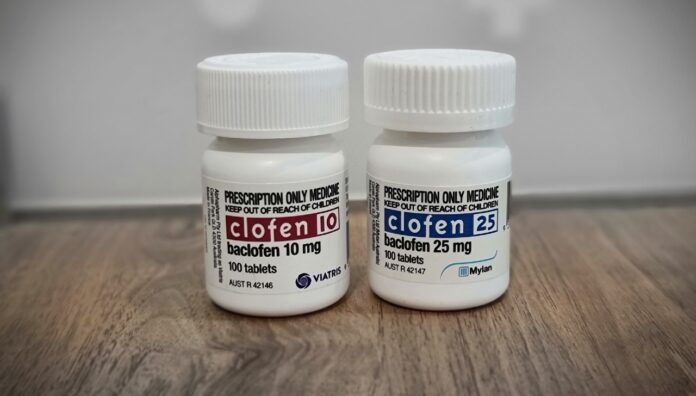
Another treatment option is baclofen, indicated for the relief of spasticity in conditions such as multiple sclerosis and spinal lesions.
In Therapeutic Guidelines, baclofen is recognised as an off-label treatment for alcohol use disorder, but is not a first-line treatment and should be used under the supervision of a specialist.
The risks of overdose are heightened when baclofen is used in high doses for off-label treatment of alcohol-use disorder, the Therapeutic Goods Administration (TGA) has warned.
Here’s what pharmacists need to be aware of to ensure the medicine is used safely.
1. Off-label use of baclofen in high doses can cause overdose and death
Up until October 2023, there were 43 cases of overdose reported to the TGA, along with two deaths linked to baclofen that were subject to coronial inquiries.
Baclofen is linked to both intentional and unintentional overdoses and deaths. The medicine can cause suicidal ideation, particularly when used in higher doses (> 80 mg/day).
Baclofen was involved in 31 deaths reported to the Coroners Court of Victoria between 2009 and 2018. Over half (n = 17) of these deaths were linked to intentional overdoses.
One of these, involving a 36-year-old woman in 2015, was initially investigated as a homicide due to multiple traumatic injuries.
Several medicines other than baclofen were found in her system – including citalopram, quetiapine, morphine, codeine, nordiazepam, oxazepam and temazepam. But the forensic pathologist advised that the elevated levels of baclofen (4.8 mg/L) were enough to cause death alone. The coroner ruled that the injuries were caused by a series of falls resulting from the baclofen overdose.
A 64-year-old patient died in 2020, with both alcohol and baclofen found in her system.
2. Different indications = different doses
When prescribed as indicated to relieve spasms, cramping, and tightness of muscles, baclofen is commonly taken at doses of 5–10 mg three times per day, but may be used in higher doses, said Professor Suzanne Nielsen MPS, Deputy Director of the Monash Addiction Research Centre in Melbourne.

As baclofen is prescribed off-label for alcohol use disorder, there are no licensed doses for this indication.
‘In a number of randomised control trials, baclofen is used in doses of 30 mg per day for alcohol use disorder, though some studies test higher doses,’ she said.
‘If you start to see doses above 30 mg a day, contact the prescriber to ensure it’s intentional, as there are greater safety concerns with the use of higher doses.’
3. Know the symptoms of baclofen toxicity
Signs of baclofen toxicity include:
- confusion
- delirium
- central nervous system (CNS) and respiratory depression
- hypotonia
- flaccid paralysis
- haemodynamic instability.
‘Pharmacists should keep an eye out [for those] who appear sedated, lethargic, or who are slurring their speech or displaying any signs of confusion, which could indicate overuse or more severe adverse effects,’ she said.
These signs could also indicate sedation from other agents, which could pose a risk to patients using baclofen.
4. Mitigate risks from other CNS depressants: RTPM can help
If pharmacists are concerned a patient is overusing baclofen or have other concerns about patient safety, they could check the patient’s dispensing history, My Health Record and real-time prescription monitoring systems to confirm if there is a risk from combining baclofen with other sedative medicines.
Where other CNS depressants are prescribed, ensure there has been an assessment of the safety of the combination by:
- checking there is still an indication for all other CNS depressant medicines
- ensuring these medicines provide benefits to the patient
- determining if deprescribing other CNS depressant medicines has been considered.
‘We often see additional medicines started before other medicines that haven’t been working are stopped,’ said Prof Nielsen. ‘So it represents good clinical care to look at all the medicines a patient is prescribed and assess if they are still needed.’
5. Engage in non-judgemental conversations with patients
If signs of misuse or dependence are detected, initiate a non-judgemental conversation with the patient to understand how they’re using their medicines and if they are still receiving clinical benefits.
Possible questions include:
- have you found yourself needing to take a higher dose of baclofen to get the same results?
- do you find the medicine provides relief from other symptoms such as stress or to help you sleep?
Open-ended questions may elicit more information, such as ‘can you tell me about how you are taking your baclofen?’
If baclofen is used off-label for alcohol use, ask the patient how their treatment for alcohol use disorder is going and what their goals of therapy are.
‘If they’ve started drinking [alcohol] again – make sure they go back and talk to the prescriber about it,’ said Prof Nielsen.
Ensure patients understand that the medicine is only safe and effective when used at the prescribed dose the prescriber deems appropriate.
‘If patients are taking higher doses, explain that it can increase the risk of side effects and overdose, particularly in combination with other CNS depressant medicines.’
There are concerns with suicide and suicide-related events in patients who use baclofen. To be able to best assess patients’ suicidal risk, pharmacists should undertake Mental Health First Aid training. Patients should also be referred to Lifeline if needed.
6. When in doubt, check in with prescribers
One role of pharmacists is to identify where medications may or may not be safe and appropriate, said Prof Nielsen.
‘If you encounter any doses of baclofen outside the normal therapeutic range, contact the prescriber to understand the rationale behind it and to check that a reasonable number of measures are in place to protect the patient’s safety,’ she said.
If there are any concerns about the patient’s mental health, pharmacists should contact the prescriber to explain the change in the patient’s presentation.
‘Where there is some clinical benefit of baclofen to the patient, but there are concerns about how the patient is managing their medicines, look at options such as staged supply, in collaboration with prescribers,’ said Prof Nielsen.
‘If the prescriber assesses that there isn’t a benefit, it might be worth tapering a patient off the medicine.’
7. Document everything
If baclofen is supplied early or the patient is using more than expected, ensure there is a note in the patient’s clinical file confirming:
- the issues have been discussed with the prescriber, and the outcome of this discussion
- the reason for resupply
- other steps that have been taken to ensure the patient’s safety.
‘If there are signs the patient is at risk, document the steps you’ve taken to assess and mitigate that risk,’ said Prof Nielsen.
‘Simply resupplying when it appears the patient is escalating their use of baclofen without making those notes puts pharmacists at risk should something happen to the patient.’



 Pharmacists have always prescribed, but they have the potential to prescribe much more
Pharmacists have always prescribed, but they have the potential to prescribe much more


 Sponsorship information
Sponsorship information


 Talking to patients who have questions
Talking to patients who have questions