With medicines being used more often than ever to treat mental health conditions, pharmacists’ quality use of medicines (QUM) expertise is vital to optimising therapy and preventing harm, says PSA’s newest medicine safety report.
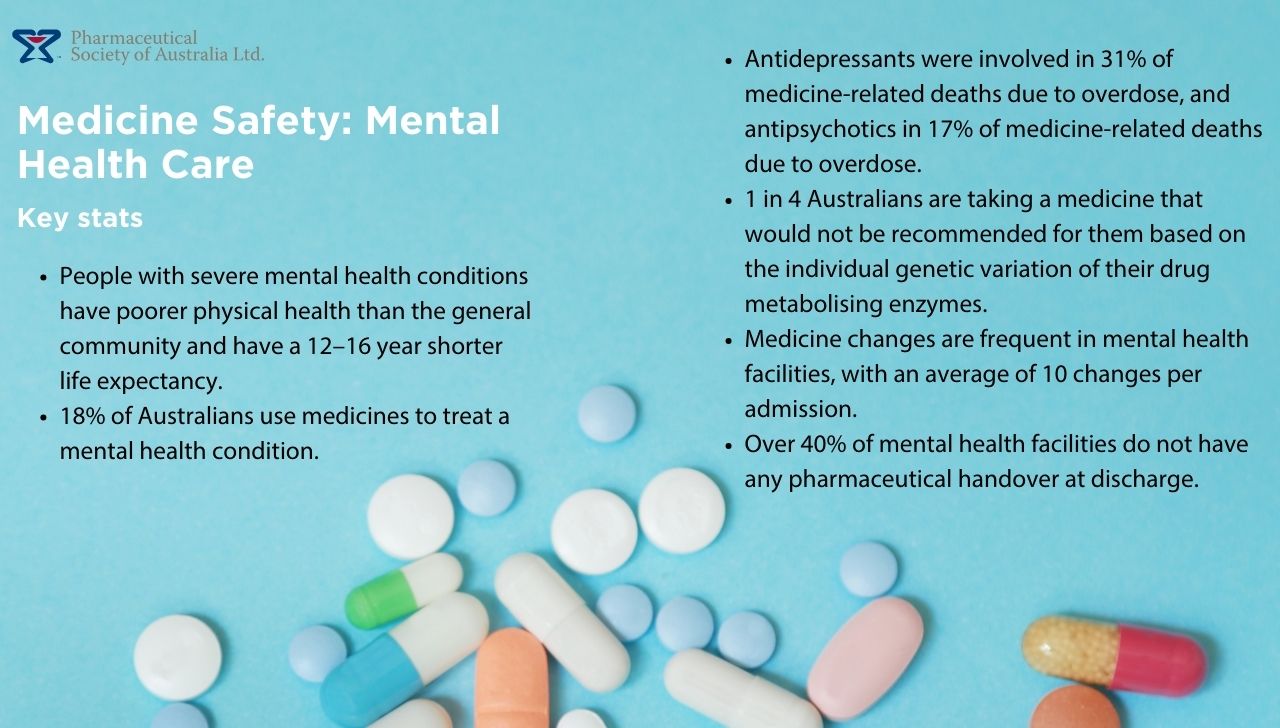
One in two Australians will experience a mental health condition in their lifetime. With mental ill health on the rise, prescriptions for mental health medicines are soaring.
Almost one fifth of Australians (14.7 million, or 18%) filled a prescription for a medicine used to treat a mental health condition in 2021-2022. Yet there is a lack of QUM oversight from pharmacists to ensure these medicines are used appropriately and safely, found PSA’s Medicine Safety: Mental Health Care report, launched today (22 November 2023).
 Wherever medicines are used there is a risk of medicine misadventure, said PSA National President Dr Fei Sim FPS.
Wherever medicines are used there is a risk of medicine misadventure, said PSA National President Dr Fei Sim FPS.
‘Too often we hear of people stopping treatment altogether because of the effects of these medicines,’ she said. ‘This is where we believe there is significant opportunity for investment in pharmacist services to help support the safe and effective use of medicines.’
Patients using medicines for mental health conditions need access to pharmacists’ medicines expertise across the spectrum of care – whether in hospitals, community settings or private clinics.
The report’s recommendations, detailed below, address gaps in care across these junctures to ensure a movement away from the ‘set-and-forget’ approach that people using mental health medicines too often experience.
 ‘This is about ensuring patients have the support they need to get the most out of their medicines safely and effectively,’ said Dr Sim.
‘This is about ensuring patients have the support they need to get the most out of their medicines safely and effectively,’ said Dr Sim.
1. Upskilling pharmacy teams in emergency care
All members of the pharmacy team should receive funded Mental Health First Aid training. This includes pharmacists and support staff across all practice settings.
Equipping pharmacy teams with the right skill set will both help to reduce stigma and ensure an appropriate response to mental health challenges.
2. Timely screening to facilitate diagnosis
Early intervention in mental health conditions is key. As community pharmacists are the most accessible healthcare professionals, funding a mental health screening program using validated screening tools and evidence-based risk assessment methods will facilitate early intervention for people experiencing mental health symptoms. This will help to ensure referral to an appropriate health practitioner or service provider for further investigation and formal diagnosis.
3. Tailored support for patients starting new medicines
Implementation of a program that funds community pharmacists to provide three Mental Health Medicines Consultation Services will help to ensure patients on new and existing mental health medicines benefit from bespoke support.
4. Addressing overdose risk
To prevent harm or death from medicine overdose, community pharmacy services such as dose administration aids and staged supply should be promoted and funded for at-risk patients living with a mental health condition.
5. Testing to find the right therapy
A patient’s genetic profile can determine how effective a medicine will be and/or if adverse effects will be encountered. Funding for pharmacogenomic testing in primary care, including identification of patients who would benefit from this service, could help to avoid use of ineffective medicines to treat mental health conditions.
6. Activating credentialed pharmacists
Mental health service providers, such as community health services and private mental health clinics, should receive funding to access skilled services provided by credentialed pharmacists. These could include:
- New mental health medicine support service, with consultations addressing medicine-related problems or adverse effects, whether the patient’s treatment goals are being met, and providing regular monitoring and review over the first year of therapy.
- Physical health and medicine support service that allows better management of comorbidities. For example, blood glucose measurement, blood pressure monitoring, weight management advice, smoking cessation services, and chronic disease medicines advice.
- Medicines monitoring and pharmacovigilance program to identify adverse effects and support patients on mental health medicines beyond the 12-month mark. Services could include periodic review of medicines and dose adjustments such as tapering, where appropriate.
7. Ongoing medication management reviews
People on mental health medicines should have access to medication management reviews every 6 months. This includes people living in residential aged care facilities or those receiving disability care services.
8. Medicines stewardship in mental health wards
Pharmacists should be rostered on 7 days a week in all hospital mental health wards to participate in multidisciplinary teams and provide after-hours mental health pharmacist services. This will help to embed medicines stewardship and ensure adequate resourcing for clinical handover.
9. Improving transitions of care
Formalising transitions of care pharmacist services will help to reduce error incidents that could lead to medicine misadventure, including duplication of therapy, continuation of medicines which have been stopped, and reintroducing medicines deemed ineffective or unsafe for the patient.
Government support for change
As a pharmacist who once worked in acute adult inpatient services, Assistant Minister for Mental Health and Suicide Prevention and Assistant Minister for Rural and Regional Health, Emma McBride MP, believes the report will be ‘influential’ in improving patient care.
‘This is a timely report on the importance of medication safety in mental health given the prevalence of common mental health disorders and the medications often prescribed as part of treatment and care,’ she said.
‘The report also highlights the vital role pharmacists play – across settings – to improve safety and importantly reduce harm.’
Read the full report here:








 This article was sponsored and developed in collaboration with PSA and Carers NSW[/caption]
However, pharmacists may perceive medication errors or non-adherence as a carer’s inability to fulfil this role,
This article was sponsored and developed in collaboration with PSA and Carers NSW[/caption]
However, pharmacists may perceive medication errors or non-adherence as a carer’s inability to fulfil this role,