

td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28164
[post_author] => 3410
[post_date] => 2024-11-13 12:50:58
[post_date_gmt] => 2024-11-13 01:50:58
[post_content] => The Therapeutic Goods Administration (TGA) has worked with Phenergan manufacturer Sanofi to develop a new contraindication for the medicine in children under 6.
The decision to restrict use of the medicine in this age cohort – commonly used to treat allergies, travel sickness and nausea – is based on a thorough evaluation of new scientific evidence that the risks outweigh the benefits, a spokesperson for Sanofi told Australian Pharmacist.
‘Following recent evaluations made by Sanofi Consumer Healthcare Pty Ltd, including a benefit-risk assessment, the research has shown a causal association between promethazine and safety concerns,’ said this spokesperson.
The sponsor-initiated update was prompted by advice from the TGA Advisory Committee on Medicines (ACM) – first-generation oral sedating antihistamines – do not use in children, said a spokesperson from the TGA.
‘Further review by the sponsor of cumulative safety data in children 2 to 5 years of age demonstrated sufficient evidence of a causal association between promethazine and psychiatric and central nervous system adverse events in this age group,’ the TGA spokesperson told AP.
The contraindication comes after Medsafe, the New Zealand Medicines and Medical Devices Safety Authority, moved to contraindicate the use of the medicine in children under 6 due to the potential for fatal respiratory depression, psychiatric and central nervous system (CNS) events.
AP understands that the contraindication will affect other products. A spokesperson for AFT said a variation has been submitted to update the product information and label on Allersoothe Elixir with a change to the age indication from children 2 years and older to children 6 years and older. This submission is pending approval.
Will the packaging change?
Not immediately.
New labels for promethazine-containing products will be rolled out in 2025 due to production and logistics lead times, said the Sanofi spokesperson.
‘No immediate action is required regarding current stock. There is no need to set aside existing medications, as this communication does not constitute a recall,’ said the spokesperson. ‘Similarly, the revised labels do not create any changes in the ordering process.
The product information for Phenergan has been updated and is available here.
What should pharmacists do if they get a Phenergan script for an 18 month old infant?
The use of promethazine in children under 6 years of age is now both contraindicated and off label, said Peter Guthrey MPS, PSA Senior Pharmacist – strategic policy.
‘This means that if you choose to dispense, both the prescriber and dispenser carry the full indemnity risk, and you need to get the patient to provide informed consent,’ he said.
Should a parent present with a script for promethazine for use in a child under 6 years of age, pharmacists should contact the prescriber to discuss the risks and benefits, noting that it's contraindicated.
Is there any situation where it would be appropriate to dispense Phenergan to a young child?
It would need to be a pretty compelling case, where the benefit to a child outweighed the risk of respiratory depression, psychiatric or CNS events , said Mr Guthrey.
‘Given it’s a documented contraindication, it'd be pretty hard to demonstrate the medicine is ‘‘safe and therapeutically appropriate’’,’ he said.
‘It is going to be difficult to find a situation where supply is clinically justified and pharmacists have met their obligations to patient safety.’
What about prescribing Phenergan as a Schedule 3 medicine?
If a parent requests promethazine as a Schedule 3 medicine for someone under the age of 6 years, generally alternate products or advice for treatment should be provided following a discussion.
‘While a pharmacist prescribing promethazine as a Pharmacist Only Medicine is lawful for children aged 2-5 years, it is still contraindicated,’ said Mr Guthrey. ‘There would be very few, if any, situations where prescribing the medicine where contraindicated would be warranted.’
What about phenylephrine?
There are some combination phenylephrine products indicated for children under 6 years of age for nasal congestion. However, there is plenty of evidence showing that oral phenylephrine products are ineffective as a nasal decongestant.
In fact, the United States Food and Drug Administration (FDA) recently announced it will move to ban oral phenylephrine products because they simply don't work.
‘Based on our review of available data, and consistent with the advice of the advisory committee, we are taking this next step in the process to propose removing oral phenylephrine because it is not effective as a nasal decongestant,’ said Patrizia Cavazzoni, M.D., director of the FDA’s Center for Drug Evaluation and Research .
While a spokesperson for the TGA told Australian Pharmacist back in July that there are ‘no plans’ to review the effectiveness of oral phenylephrine, it will continue to monitor the outcomes of the FDA review.
What advice should pharmacists provide?
For children with allergies, non-sedating histamines are first line.
The best thing parents can do when a child under 6 years of age has cough or cold symptoms is to wait it out, with a review by a medical practitioner when appropriate.
‘It's about reassurance to parents that the cough in itself isn't harmful, and that kids don’t always need medicines for a cold – they need time and supportive therapy,’ said Mr Guthrey.
It’s important that pharmacists give parents confidence that they're doing the right thing by not treating the cough, and providing symptomatic relief for fever and chills, and ensuring they are appropriately counselled on when review by a medical practitioner may be appropriate.
For more information, refer to the Australian Pharmaceutical Formulary and Handbook treatment guidelines on:
[post_title] => Do not supply Phenergan to children under 6, manufacturer warns
[post_excerpt] => The TGA has worked with Phenergan manufacturer Sanofi to develop a new contraindication for the medicine in children under 6.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => do-not-supply-phenergan-to-children-under-6-manufacturer-warns
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-13 16:15:31
[post_modified_gmt] => 2024-11-13 05:15:31
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28164
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Do not supply Phenergan to children under 6, manufacturer warns
[title] => Do not supply Phenergan to children under 6, manufacturer warns
[href] => https://www.australianpharmacist.com.au/do-not-supply-phenergan-to-children-under-6-manufacturer-warns/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28167
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28142
[post_author] => 3410
[post_date] => 2024-11-11 15:55:46
[post_date_gmt] => 2024-11-11 04:55:46
[post_content] => With cases of Respiratory syncytial virus (RSV) spiking this year, the federal government announced yesterday (10 November) that free vaccination would be offered to eligible pregnant people and babies.
Before the 2025 winter season, the RSV vaccine will be available under the National Immunisation Program (NIP) for all people in the third trimester of pregnancy via the Australian Infant RSV Immunisation Program.
Which RSV vaccines will pharmacists administer?
The RSV immunisation program will offer two Therapeutic Goods Administration approved protections against severe RSV.
Pharmacists can administer the maternal vaccine, Abrysvo, to pregnant women between 28-36 weeks of gestation.
Maternal vaccination provides early protection for newborn children by reducing the risk of severe RSV disease in infants under 6 months of age by around 70%, a spokesperson from the Department of Health and Aged Care told Australian Pharmacist.
‘This is [through] passive protection by transplacental transfer of RSV-specific antibodies from the mother to the foetus during pregnancy.’
How popular will it be?
Federal Minister for Health and Aged Care Mark Butler said the RSV vaccine rollout has been modelled on the whooping cough vaccine in pregnant women, which is administered at around the same time and has an uptake rate of around 80%.
‘Maternal vaccination provides early protection for newborn children by reducing the risk of severe RSV disease in infants under 6 months of age by around 70%.'
The Department of Health and Aged Care
‘So we have good confidence that there will be a significant uptake of this maternal vaccine by pregnant Australian women,’ he added.
What is covered for pharmacists under the NIP?
According to the Department of Health and Aged Care, both the cost of the maternal RSV vaccine (Abrysvo) and the vaccine administration fee will be covered under the NIP and The National Immunisation Program Vaccinations in Pharmacy (NIPVIP) Program.
Abrysvo NIP vaccine stock will also be available to community pharmacists, said the spokesperson.
What about protection for neonates?
Access has also widened for more babies to receive a protection against RSV soon after birth, particularly those whose mother did not opt to have the vaccine during pregnancy.
Beyfortus (nirsevimab), an antibody therapy for the prevention of RSV-related lower respiratory tract disease, will be available in hospitals, immunisation clinics and general practices for infants before or during their first RSV season. Children up to 24 months of age who remain vulnerable to severe RSV disease throughout their second RSV season can also access the vaccine.
‘Beyfortus is a monoclonal antibody treatment which is administered to babies by injection,’ said Minister Butler. ‘[It can be received] immediately after birth … if their mother has not been vaccinated against RSV.’
Why did the government decide to take action against RSV?
Australia recorded the highest ever number of RSV cases this year, with 165,910 reported notifications.
Most cases were recorded in the 0–4 age cohort, among whom RSV can be fatal, and is the leading cause of hospitalisation for Australian children under five years of age.
The Australian Immunisation Foundation estimates that around 12,000 Australian babies aged 12 months or younger are admitted to hospital with RSV annually. Around 25% of these children will require intensive care.
The inclusion of an RSV vaccine in the NIP is an important step to protect newborn children and infants from severe RSV infection, said the spokesperson.
‘The highest rate of RSV-related hospitalisations is in infants during their first few months of life,’ said the spokesperson.
‘Infants with medical risk factors, such as being born very [premature], under 32 weeks gestational age, have an increased risk of severe disease.
‘Up to 80% of infants who are hospitalised due to RSV are otherwise healthy children with no predisposing conditions.’
What’s the expected impact?
The Immunisation Foundation of Australia has estimated that the nationwide availability of new RSV immunisations will help to keep 10,000 infants out of hospital with related bronchiolitis or pneumonia each year.
‘The immunisations being funded in Australia protect babies against severe RSV and have been shown to slash hospitalisation rates by up to 90 per cent,’ said Catherine Hughes AM, Founder and Director of the Immunisation Foundation of Australia.
Western Australia was the first state to implement an infant RSV immunisation program with Beyfortus. More than 23,000 infants received RSV protection this year, resulting in up to 84% fewer hospitalisations in immunised newborns compared to those who were not RSV protected. In Queensland, where a statewide infant RSV immunisation program commenced in April 2024, similar results were observed.
‘The exceptional results in Western Australia and Queensland contrast sharply with other parts of Australia where hospitals were overwhelmed by babies struggling to breathe due to severe RSV,’ she said.
Will older patients be able to receive the RSV vaccine under the NIP?
No. Well at least, not yet.
Vaccines can only be listed on the NIP after a positive recommendation from the Pharmaceutical Benefits Advisory Committee’s (PBAC) as required by the National Health Act 1953, said the spokesperson.
‘Several vaccine sponsors have made submissions in relation to RSV vaccines for older populations to the PBAC to consider for NIP listing,’ said the spokesperson.
‘The outcomes of these meetings will inform future government considerations regarding the potential listing of RSV vaccines on the NIP for older Australians.’
While a positive PBAC recommendation is an essential requirement in the NIP-listing process, other steps need to be completed before a vaccine can be given final approval for NIP listing, said the spokesperson.
‘These include negotiations with the relevant pharmaceutical company, finalisation of conditions for listing, quality and availability checks and final consideration by the government,’ said the spokesperson. ‘These considerations and decisions of government cannot be preempted.’
[post_title] => Government-funded RSV vaccines to protect infants from severe disease
[post_excerpt] => With cases of RSV spiking in 2024, the federal government announced free vaccination would be offered to eligible pregnant people and babies.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => government-funded-rsv-vaccines-to-protect-infants-from-severe-disease
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-13 13:26:32
[post_modified_gmt] => 2024-11-13 02:26:32
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28142
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Government-funded RSV vaccines to protect infants from severe disease
[title] => Government-funded RSV vaccines to protect infants from severe disease
[href] => https://www.australianpharmacist.com.au/government-funded-rsv-vaccines-to-protect-infants-from-severe-disease/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28146
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28134
[post_author] => 9164
[post_date] => 2024-11-11 12:48:48
[post_date_gmt] => 2024-11-11 01:48:48
[post_content] => Pharmacists and migrant community leaders, Sobia Hashmi MPS and Irfan Hashmi MPS, are the 2025 Local Heroes for South Australia, receiving their award on Saturday night in a ceremony in Adelaide.
The local heroes category of these Australia Day awards recognise role models who encourage others to be active in their own communities and become agents of positive change for a more diverse and inclusive Australia.
Over 20 years, Sobia and husband Irfan have transformed healthcare in remote and rural communities in South Australia. They’ve established six pharmacies in areas where there were previously none – which forced people to travel long distances for life-saving medicines and primary health care.
Sobia (48) and Irfan (51) are committed to serving their diverse communities. They employ staff who collectively speak 21 languages, allowing them to reach vulnerable populations and provide culturally sensitive healthcare. In 2020, they partnered with government to provide 24 free influenza vaccine clinics in outreach settings, providing 1200 vaccines to vulnerable people in South Australia.
Reflecting on the awards, Irfan and Sobia told Australian Pharmacist that the award was a celebration of the collective efforts of everyone who has been with them along the way, including their family, friends, colleagues, and the broader community.
‘To every individual who believed in us, who encouraged us to reach higher, and who shared in our vision of uplifting others, thank you. Your unwavering support drives us to do more, reach further, and connect deeper with those around us,’ they said.
Sobia and Irfan also reflected on the importance of community.
‘Together, we are stronger. Together, we make a difference. And together, let’s continue to build a healthier, more inclusive South Australia for all. This is just the beginning, and we are excited for the journey ahead,’ they said.
‘We are truly honoured and humbled to be named the 2025 Australian of the Year Award – Local Hero in SA recipients. This recognition strengthens our commitment to making a positive impact as pharmacists and community leaders, and it inspires us to continue serving the vibrant multicultural community that we call home.’
The couple have mentored countless intern pharmacists from overseas, coordinating multilingual education and outreach initiatives to help pharmacists enter the much-needed workforce in regional Australia. They host a free weekly webinar series, which has assisted 4,000 overseas pharmacists in passing their registration exams in the last 12 months alone.
Irfan previously was recognised as PSA’s 2009 South Australian Pharmacist of the Year.
[post_title] => Two pharmacists win state Australian of the Year 2025 award
[post_excerpt] => Sobia Hashmi MPS and Irfan Hashmi MPS will attend the Australian of the Year awards as finalists for the national local heroes title.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => two-pharmacists-win-state-australian-of-the-year-2025-award
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-13 13:26:46
[post_modified_gmt] => 2024-11-13 02:26:46
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28134
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Two pharmacists win state Australian of the Year 2025 award
[title] => Two pharmacists win state Australian of the Year 2025 award
[href] => https://www.australianpharmacist.com.au/two-pharmacists-win-state-australian-of-the-year-2025-award/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28140
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 27932
[post_author] => 235
[post_date] => 2024-11-07 00:53:00
[post_date_gmt] => 2024-11-06 13:53:00
[post_content] => A megatrend has begun in medicines. The increasingly large and full fridges found in pharmacies stand as a testament to the growing prevalence of injectable medicines – and are a sign of things to come.
In the near future, many daily tablets may be replaced with periodic appointments to have a medicine administered by injection.
The injectables are coming
Options for injectables and other non-oral dose forms such as patches, gels and sprays are rapidly growing, with these increasingly replacing medicinal therapies delivered through swallowing tablets, capsules or liquids. Pharmacists will recognise these examples.
Prolia (denosumab), which has been registered for the treatment of osteoporosis in Australia since 2010, offers a glimpse of the future, replacing daily or weekly tablets with biannual injections.1 Similarly, the relatively new cholesterol-lowering drug Leqvio (inclisiran) is administered every 6 months as a maintenance dose, after the initial induction doses, offering a new route for lipid modifying therapy.2
And Eli Lilly has a new US Food and Drug Administration-approved injectable, Kisunla (donanemab-azbt), coming out for the treatment of Alzheimer’s disease (AD).3 Delivered by infusion every 4 weeks, the drug works by targeting deposits of amyloid plaque in the brain, which is a key indicator of the presence of the debilitating, ultimately fatal brain disease.
Last month, one of the world leaders in AD research, Professor Colin Masters of The Florey Institute of Neuroscience and Mental Health in Melbourne, told neurologists and healthcare workers who treat patients with progressive neurodegenerative diseases of promising results from the Roche Dominant Inherited Alzheimer’s Network (DIAN) trial of the monoclonal antibody gantenerumab. Roche’s “Brain Shuttle” technology is now being used to cross the blood-brain barrier and then clear amyloid plaque aggregation with a newer generation, bio-specific, monoclonal antibody called trontinemab.
Prof Masters told a Creutzfeldt-Jakob Disease Support Group Network (CJDSGN)workshop on CJD and other prion diseases that early results from a trial of trontinemab are currently in pre-press in The Lancet.⁴

It’s also hoped, he says, that current intravenous AD drug models may evolve to be delivered subcutaneously via an autoinjector by patients at home.
Perhaps most revolutionary, however, are the advancements in HIV prevention. Recently, research into Gilead’s long-acting injection, lenacapavir (an agent for treatment of HIV), has shown promising results in pre-exposure prophylaxis (PrEP), and has been described as ‘the closest we have ever been to an HIV vaccine’ .⁵ At the AIDS 2024 conference in Germany in July, researchers presented their findings that twice-yearly lenacapavir demonstrated 100% efficacy for HIV prevention in cisgender women.⁶
‘The pace at which innovative, new medicines are entering the market is unprecedented,’ says Medicines Australia CEO Liz de Somer. ‘Advances in research, technology and innovation mean we can expect to see new forms of treatments – which include innovative new medicines and improved forms of existing medicines – becoming available.’
These are huge leaps forward in how health is treated, and pharmacists will need to adapt, says PSA National Board member Dr Shane Jackson FPS, community and credentialed pharmacist and lecturer in pharmacy at the University of Tasmania.
‘Medicines have always been an evolving space. Research on mRNA-delivered therapeutics has actually been around for about 20 years, and the pipeline of mRNA therapeutics is and will be a gamechanger in terms of treatment and prevention of disease in the future,’ he says.
‘What this means is that pharmacists will be needed more than ever because of their deep expertise in the use of medicines, and the term “medicines experts” will most likely evolve to “therapeutics experts”, noting the change from “medicine” to the complete management and prevention of disease.’
 New formats needed
New formats needed
One reason alternative delivery systems like injections and patches are becoming more prevalent is because they are critical for delivering new, biologically complex drugs.
As scientists have developed new treatments, they have created molecules that are too large or sensitive to be absorbed effectively through the digestive system. For example, Humira (adalimumab), the monoclonal antibody used to treat autoimmune conditions including juvenile arthritis and Crohn’s disease, is administered through subcutaneous injection because its large molecular structure would be ineffective if taken orally.⁷
Or take the testosterone transdermal delivery patch Androderm.8 Delivering testosterone directly through the skin provides a steady hormone level that can’t be achieved with oral testosterone.⁹
Technological advancements in mRNA technology, showcased in the production of COVID-19 vaccines, are also driving treatments and other preventive measures for different conditions.
‘Prior to the pandemic, mRNA-based drug products were focused primarily on treating oncology indications as opposed to infectious diseases, such as COVID-19,’ says Martin Gonzalez, Pfizer’s senior manager of product development.10
‘However, technical and scientific advancements have allowed researchers and drug developers to expand the use of mRNA to new therapeutic areas.’
For patients who inject themselves daily, there is also a growing preference for better ways to self-administer medicines. This focus on the patient has led to advances in medical devices in recent decades, introducing prefilled syringes, pens and automated electronic and infusion devices.

‘Much of the emphasis in contemporary drug design has shifted from just preserving basic quality attributes, such as safety, efficacy and potency, in a simple container,’ Mr Gonzalez says.10
‘Today’s [sterile injectable] drugs carry a more complex profile and incorporate new thinking about ways of preserving the value of the drug while also providing additional benefits, including precise, easy-to-administer delivery systems for better dose compliance.’
Improving medicine adherence
According to the World Health Organization, around 50% of patients with chronic illnesses in developed countries don’t take their medicines as prescribed.11
The rates are even lower in developing nations. There are myriad reasons for poor medicine adherence, including low health literacy, the prescription of complex drug regimens and limited access to care.12
Long-acting therapies may also be beneficial for hard-to-reach populations, such as those experiencing homelessness or substance use problems. And in the case of those living with HIV, long-acting drugs might also be useful for children, says Dr Charles Flexner, HIV expert at Johns Hopkins University. Globally, just 50% of children diagnosed with HIV are receiving treatment, in part due to a lack of drug versions made for children.13
‘With long-acting formulations, that will no longer be the case,’ Dr Flexner says.13 ‘Children will be able to use the same formulation as adults, just at a different dose.’
Breakthrough in injectable PrEPLong-acting injectables for HIV treatment and prevention are providing convenience, promoting better adherence, and helping to reduce the stigma and discrimination that might come with taking a daily pill.14 In Australia, there is currently one injectable HIV medicine listed on the Pharmaceutical Benefits Scheme (PBS) – Cabenuva (cabotegravir/rilpivirine), which requires injections every 2 months.15 Cabotegravir-LA for pre-exposure prophylaxis (PrEP) has been approved by the Therapeutic Goods Administration (TGA) but is not yet listed on the PBS,16 and lenacapavir is also TGA-approved but not PBS listed for treating multidrug-resistant HIV in combination with other antiretroviral therapy. Globally, 6-monthly injections of lenacapavir have also been trialled for PrEP, with extraordinary results. Clinical trial data released this year in a study of cisgender men, transgender men, transgender women, and nonbinary individuals who have sex with partners assigned male at birth showed that using lenacapavir results in a 96% lower HIV rate compared with the expected incidence of infection, and an 89% lower HIV rate compared with oral PrEP.17
Trials have also shown an efficacy rate of 100% among cisgender women in South Africa and Uganda.
Professor Sharon Lewin, Director of the Peter Doherty Institute for Infection and Immunity at the University of Melbourne, and immediate past president of the International AIDS Society, described the results as ‘a breakthrough advance with huge public health potential’.
‘If approved and delivered – rapidly, affordably and equitably – to those who need or want it, this long-acting tool could help accelerate global progress in HIV prevention,’ Professor Lewin said.⁶
When it comes to long-acting injectables for HIV treatment and prevention: watch this space. Clinical trial data released this year in a study of cisgender men, transgender men, transgender women, and nonbinary individuals who have sex with partners assigned male at birth showed that using lenacapavir results in a 96% lower HIV rate compared with the expected incidence of infection, and an 89% lower HIV rate compared with oral PrEP.17
Trials have also shown an efficacy rate of 100% among cisgender women in South Africa and Uganda.
Professor Sharon Lewin, Director of the Peter Doherty Institute for Infection and Immunity at the University of Melbourne, and immediate past president of the International AIDS Society, described the results as ‘a breakthrough advance with huge public health potential’.
‘If approved and delivered – rapidly, affordably and equitably – to those who need or want it, this long-acting tool could help accelerate global progress in HIV prevention,’ Professor Lewin said.⁶
When it comes to long-acting injectables for HIV treatment and prevention: watch this space. |
As more injectable medicines come onto the market, the pharmacy of the near future will need more consultation rooms and more dispensary refrigerator space.
Pharmacy practice will likely involve more direct patient care, including administering injections and managing complex treatment regimens. Those who fail to adapt, for example by not learning to inject safely, risk becoming obsolete, as the profession increasingly shifts to a more hands-on role.
‘In terms of medicines administration [by injection], this is a newish activity that pharmacists are undertaking,’ Dr Jackson points out. ‘It is becoming increasingly relevant because of a lack of access to general practice care and the acknowledgement that this activity is and has always been within the scope of practice of a pharmacist in terms of education and training.
‘Pharmacists need to ensure they are competent in terms of their training (vaccination certified, medicines administration training has been completed) and that they inform themselves of the relevant information related to each drug being administered.
 ‘In my view, it’s analogous to dispensing a new drug that you haven’t come across before. You understand the relevant information related to the drug from a safety and effectiveness point of view, you communicate with the patient regarding relevant counselling points, and you document relevant information.’
‘In my view, it’s analogous to dispensing a new drug that you haven’t come across before. You understand the relevant information related to the drug from a safety and effectiveness point of view, you communicate with the patient regarding relevant counselling points, and you document relevant information.’
But the future isn’t just about the administration of a medicine. Rather, Dr Jackson says, this is just the start of pharmacists ‘being more involved and taking more responsibility and accountability for patient care’.
‘Regulatory misunderstanding and regulatory impediments have for a long time prevented pharmacists from doing more in the prescribing, administration and review of medicines.
‘We are seeing these barriers being reduced, albeit slowly in some jurisdictions, to allow pharmacists to do more, to practise to their full scope in terms of medicines management.
‘Ideally, pharmacists should be empowering patients to better take control of their own health care. For most of the medicines we see currently, patients with appropriate support can self-administer,’ says Dr Jackson.
‘In some cases, there may be barriers in place and pharmacists may deliver regular injections for these patients. It’s a case-by-case basis with the patient at the centre of care.’
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28084
[post_author] => 3410
[post_date] => 2024-11-06 15:56:15
[post_date_gmt] => 2024-11-06 04:56:15
[post_content] => After months of anticipation, the Unleashing the potential of our health workforce – Scope of practice review was released yesterday (5 November) – with many of the key recommendations echoing the long-held concerns of the PSA and pharmacists across Australia.
Australian Pharmacist has rounded up some of the key takeouts from the report.
Pharmacists are leaving the profession at an alarming rate
Pharmacy has a high attrition rate compared with other healthcare professions. Among 19 healthcare professions, pharmacy had the fifth highest exit rate of 8.7% in 2023 – almost double that of medical professionals (4.7%).
The professions with the highest exit rates are those that face significant barriers to working to their full scope of practice, the review found.
While there are several factors that impact exit rates, allowing pharmacists to work to their full scope of practice is a crucial factor for strengthening the profession’s retention rate – improving recognition for professional skills, capability and contribution to enhance continuity of care.
‘This report really makes clear that there are all sorts of artificial, inefficient restrictions on what nurses, pharmacists, GPs, and other health professionals are allowed to do that bears no relationship to their training,’ said federal Minister for Health and Aged Care Mark Butler.
Inconsistencies in vaccine schedules for pharmacists are ‘needless’
Pharmacist vaccinators are trained in accordance with the National Immunisation Education Framework, ensuring high standards in vaccine administration and competence.
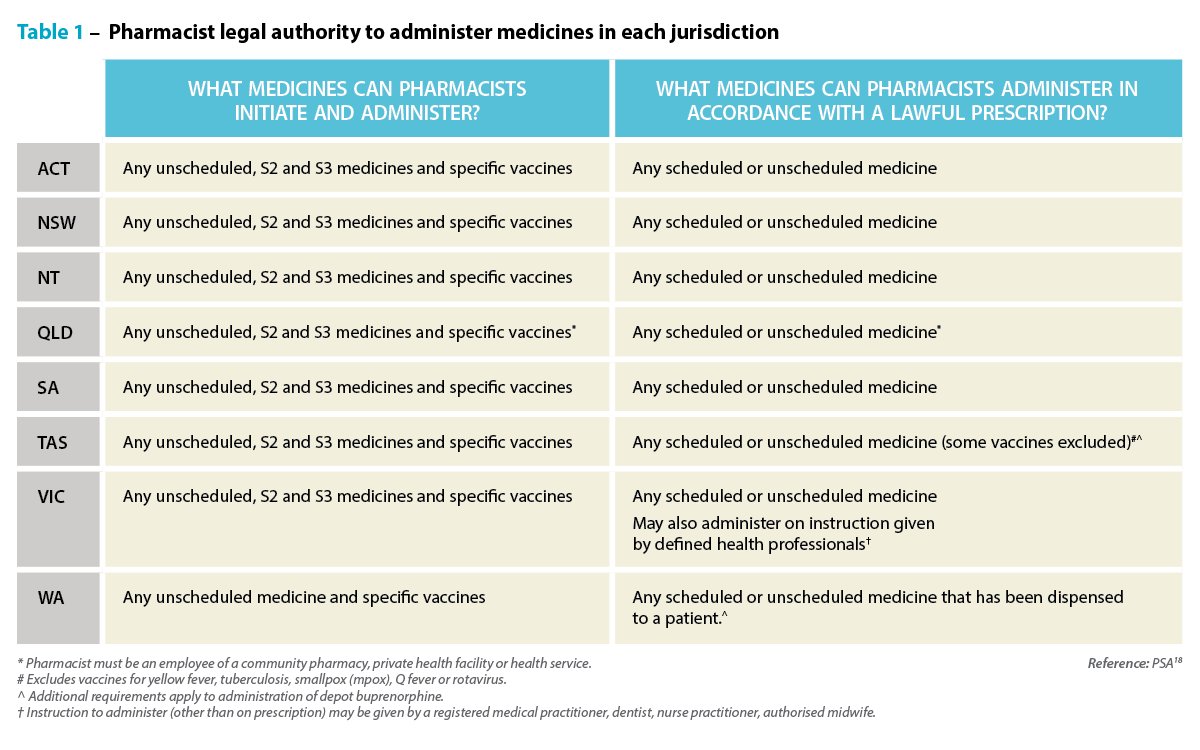
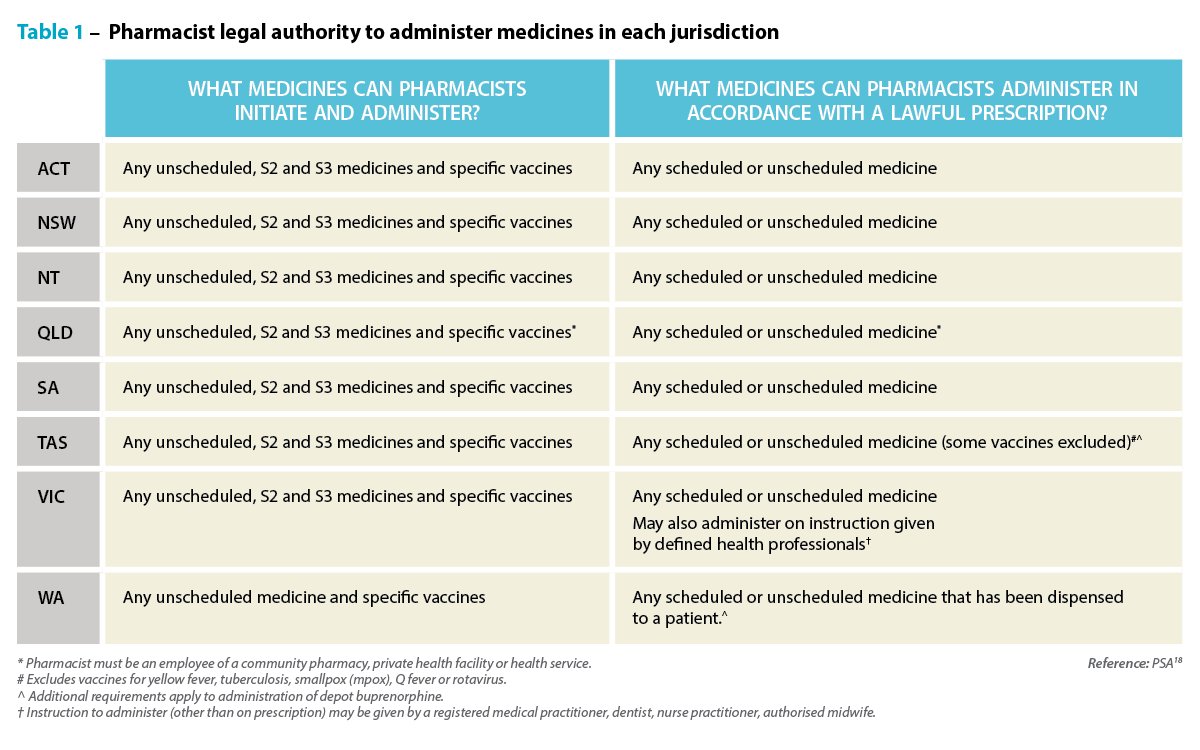
But the report found that the difference in state and territory laws dictating which vaccines can be administered by pharmacists has led to disparities in access – not only causing confusion among patients but leading to significant inefficiencies.
Legislative differences between states and territories also means that a vaccine subsidised in one region might not be covered in another.
Harmonising these regulations by reviewing Drugs and Poisons Acts would promote equitable vaccine access nationwide, allowing pharmacists’ to provide consistent healthcare services regardless of location.
Aligning funding arrangements for vaccination is also crucial, the review found. While the National Immunisation Program Vaccinations in Pharmacy (NIPVIP) provides government funding for certain vaccines, access to others depends on a mix of user-pay systems and varying jurisdictional funding – creating inconsistencies in affordability and accessibility across states and territories.
Standardising funding mechanisms would ensure subsidies are uniformly applied – making vaccinations more affordable and accessible to all Australians.
It will take some time to implement change, but there are some steps governments and regulators can take now
While some of the recommendations in the review, such as harmonising vaccination legislation, can be achieved in a timely fashion, others are sweeping reforms that will take many years, such as restructuring healthcare education – which currently impacts students and qualified pharmacists’ ability to work to their full scope.
The review recommended the Commonwealth establish a primary care workforce development program to support the development and retention of a skilled, stable, and collaborative primary care workforce through enhanced curriculum, training, placement, and career development opportunities for students, supervisors, mentors, and health professionals.
The current funding model must be overhauled
The current fee-for-service arrangement in primary care incentivises high-turnover care – with payments to providers based on the number and type of care episodes delivered.
This model limits the ability of health professionals to work to their full scope and reduces multidisciplinary collaboration – with some healthcare professionals funded for certain services while others are not, including lack of funding for pharmacists to participate in multidisciplinary case conferences.
To address this, the review recommends introducing a blended payment model to complement the fee-for-service system. This model would enable access to multidisciplinary healthcare delivered by professionals working to their full scope of practice in primary care.
An independent mechanism would be established to advise on pricing and payment levels for the blended payment, ensuring adjustments based on the risk profile of patient populations.
But it’s unlikely to be a quick fix. The review suggests the model would need to be implemented progressively over a 7-year period, beginning with priority areas such as rural and remote regions, Aboriginal Community Controlled Health Organisations, and underserviced regional and outer metropolitan areas.
Pharmacist prescribing programs should be nationally consistent
Implementing pharmacists prescribing rights has been an unnecessarily complex and prolonged process, with ad-hoc investigations, one-off reviews, and small-scale pilots.
Adopting an activity-based approach would streamline regulation for community pharmacists in prescribing medications and promote consistency across jurisdictions.
Introducing a dedicated mechanism to assess health workforce models would also fill a crucial gap, facilitating the systematic adoption of multidisciplinary primary care models that include pharmacists much like the successful models implemented in the United Kingdom.
Improved use of technology should form the backbone of scope of practice changes
A key theme in the review was the need for better use of technology across the board to expand scopes of practice and efficiencies, improving quality of care.
Potential areas for reform identified by the review include establishing access to real‑time patient information, introducing platforms for secure messaging and digital referrals and mandating participation in a multidisciplinary care team for primary care providers.
‘[We need to] improve the digital capability of a system that still uses far too many fax machines and too much paper,’ said Minister Butler.
The government will respond, in time
The government is yet to respond to the key recommendations in the report, with Minister Butler confirming he will not ‘respond to each of the ideas’.
‘We want to consider them, but a lot of them do have a lot of common sense,’ he said.
Other key stakeholders will also need to be consulted.
‘Many of the recommendations will require collaboration between the Commonwealth and state and territory governments, as well as consultation with peak professional organisations, AHPRA, patient groups, and the sector more broadly. I look forward to these discussions,’ Minister Butler added.
But PSA has called for the government to accept all 18 recommendations and put forward a plan of action now.
This review confirms PSA’s view that inconsistent regulations, unnecessary restrictions on practice, and siloed workforces are having a negative impact on patient access to quality health care, said PSA National President Associate Professor Fei Sim.
‘This report recognises the core role of pharmacies and pharmacists as primary healthcare providers and recommends a multidisciplinary approach to patient care,’ she said.
‘There is a clear alignment between Cormack’s recommendations and the actions in PSA’s vision for the pharmacy profession, Pharmacists in 2030. Both present a clear vision for the future that requires collaboration for a health system that works for patients.’
What the health sector is saying
The Australian Medical Association has said that the government ‘must resist’ changes to scope of practice, maintaining its position for even more investment into general practice.
Meanwhile, the Royal Australian College of GPs said the recommendations, if implemented, would ‘raid Medicare’, setting up for a ‘two-tiered health system where those who can afford to see a GP will, and those who can’t, don’t.’
But the Australian Nursing and Midwifery Federation said the review allows highly-trained health professionals to best utilise their skills, education and experience, allowing for the delivery of integrated, quality healthcare services across the community.
Support also came from the National Rural Health Alliance, who welcomed the recommendations that seek to address some of the ‘inequalities faced by rural Australians when it comes to accessing healthcare.’
Outside of the health sector, the Business Council of Australia also welcomed the report, citing improving ‘productivity, patient experience and workforce satisfaction’ as necessary to a sustainable health system.
[post_title] => Key recommendations to strengthen pharmacists’ role in healthcare
[post_excerpt] => The scope of practice review recommends sweeping legislative change and solutions to funding challenges to improve healthcare services.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => key-recommendation-to-strengthen-pharmacists-role-in-healthcare
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-06 17:01:11
[post_modified_gmt] => 2024-11-06 06:01:11
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28084
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Key recommendations to strengthen pharmacists’ role in healthcare
[title] => Key recommendations to strengthen pharmacists’ role in healthcare
[href] => https://www.australianpharmacist.com.au/key-recommendation-to-strengthen-pharmacists-role-in-healthcare/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28086
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28164
[post_author] => 3410
[post_date] => 2024-11-13 12:50:58
[post_date_gmt] => 2024-11-13 01:50:58
[post_content] => The Therapeutic Goods Administration (TGA) has worked with Phenergan manufacturer Sanofi to develop a new contraindication for the medicine in children under 6.
The decision to restrict use of the medicine in this age cohort – commonly used to treat allergies, travel sickness and nausea – is based on a thorough evaluation of new scientific evidence that the risks outweigh the benefits, a spokesperson for Sanofi told Australian Pharmacist.
‘Following recent evaluations made by Sanofi Consumer Healthcare Pty Ltd, including a benefit-risk assessment, the research has shown a causal association between promethazine and safety concerns,’ said this spokesperson.
The sponsor-initiated update was prompted by advice from the TGA Advisory Committee on Medicines (ACM) – first-generation oral sedating antihistamines – do not use in children, said a spokesperson from the TGA.
‘Further review by the sponsor of cumulative safety data in children 2 to 5 years of age demonstrated sufficient evidence of a causal association between promethazine and psychiatric and central nervous system adverse events in this age group,’ the TGA spokesperson told AP.
The contraindication comes after Medsafe, the New Zealand Medicines and Medical Devices Safety Authority, moved to contraindicate the use of the medicine in children under 6 due to the potential for fatal respiratory depression, psychiatric and central nervous system (CNS) events.
AP understands that the contraindication will affect other products. A spokesperson for AFT said a variation has been submitted to update the product information and label on Allersoothe Elixir with a change to the age indication from children 2 years and older to children 6 years and older. This submission is pending approval.
Will the packaging change?
Not immediately.
New labels for promethazine-containing products will be rolled out in 2025 due to production and logistics lead times, said the Sanofi spokesperson.
‘No immediate action is required regarding current stock. There is no need to set aside existing medications, as this communication does not constitute a recall,’ said the spokesperson. ‘Similarly, the revised labels do not create any changes in the ordering process.
The product information for Phenergan has been updated and is available here.
What should pharmacists do if they get a Phenergan script for an 18 month old infant?
The use of promethazine in children under 6 years of age is now both contraindicated and off label, said Peter Guthrey MPS, PSA Senior Pharmacist – strategic policy.
‘This means that if you choose to dispense, both the prescriber and dispenser carry the full indemnity risk, and you need to get the patient to provide informed consent,’ he said.
Should a parent present with a script for promethazine for use in a child under 6 years of age, pharmacists should contact the prescriber to discuss the risks and benefits, noting that it's contraindicated.
Is there any situation where it would be appropriate to dispense Phenergan to a young child?
It would need to be a pretty compelling case, where the benefit to a child outweighed the risk of respiratory depression, psychiatric or CNS events , said Mr Guthrey.
‘Given it’s a documented contraindication, it'd be pretty hard to demonstrate the medicine is ‘‘safe and therapeutically appropriate’’,’ he said.
‘It is going to be difficult to find a situation where supply is clinically justified and pharmacists have met their obligations to patient safety.’
What about prescribing Phenergan as a Schedule 3 medicine?
If a parent requests promethazine as a Schedule 3 medicine for someone under the age of 6 years, generally alternate products or advice for treatment should be provided following a discussion.
‘While a pharmacist prescribing promethazine as a Pharmacist Only Medicine is lawful for children aged 2-5 years, it is still contraindicated,’ said Mr Guthrey. ‘There would be very few, if any, situations where prescribing the medicine where contraindicated would be warranted.’
What about phenylephrine?
There are some combination phenylephrine products indicated for children under 6 years of age for nasal congestion. However, there is plenty of evidence showing that oral phenylephrine products are ineffective as a nasal decongestant.
In fact, the United States Food and Drug Administration (FDA) recently announced it will move to ban oral phenylephrine products because they simply don't work.
‘Based on our review of available data, and consistent with the advice of the advisory committee, we are taking this next step in the process to propose removing oral phenylephrine because it is not effective as a nasal decongestant,’ said Patrizia Cavazzoni, M.D., director of the FDA’s Center for Drug Evaluation and Research .
While a spokesperson for the TGA told Australian Pharmacist back in July that there are ‘no plans’ to review the effectiveness of oral phenylephrine, it will continue to monitor the outcomes of the FDA review.
What advice should pharmacists provide?
For children with allergies, non-sedating histamines are first line.
The best thing parents can do when a child under 6 years of age has cough or cold symptoms is to wait it out, with a review by a medical practitioner when appropriate.
‘It's about reassurance to parents that the cough in itself isn't harmful, and that kids don’t always need medicines for a cold – they need time and supportive therapy,’ said Mr Guthrey.
It’s important that pharmacists give parents confidence that they're doing the right thing by not treating the cough, and providing symptomatic relief for fever and chills, and ensuring they are appropriately counselled on when review by a medical practitioner may be appropriate.
For more information, refer to the Australian Pharmaceutical Formulary and Handbook treatment guidelines on:
[post_title] => Do not supply Phenergan to children under 6, manufacturer warns
[post_excerpt] => The TGA has worked with Phenergan manufacturer Sanofi to develop a new contraindication for the medicine in children under 6.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => do-not-supply-phenergan-to-children-under-6-manufacturer-warns
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-13 16:15:31
[post_modified_gmt] => 2024-11-13 05:15:31
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28164
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Do not supply Phenergan to children under 6, manufacturer warns
[title] => Do not supply Phenergan to children under 6, manufacturer warns
[href] => https://www.australianpharmacist.com.au/do-not-supply-phenergan-to-children-under-6-manufacturer-warns/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28167
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28142
[post_author] => 3410
[post_date] => 2024-11-11 15:55:46
[post_date_gmt] => 2024-11-11 04:55:46
[post_content] => With cases of Respiratory syncytial virus (RSV) spiking this year, the federal government announced yesterday (10 November) that free vaccination would be offered to eligible pregnant people and babies.
Before the 2025 winter season, the RSV vaccine will be available under the National Immunisation Program (NIP) for all people in the third trimester of pregnancy via the Australian Infant RSV Immunisation Program.
Which RSV vaccines will pharmacists administer?
The RSV immunisation program will offer two Therapeutic Goods Administration approved protections against severe RSV.
Pharmacists can administer the maternal vaccine, Abrysvo, to pregnant women between 28-36 weeks of gestation.
Maternal vaccination provides early protection for newborn children by reducing the risk of severe RSV disease in infants under 6 months of age by around 70%, a spokesperson from the Department of Health and Aged Care told Australian Pharmacist.
‘This is [through] passive protection by transplacental transfer of RSV-specific antibodies from the mother to the foetus during pregnancy.’
How popular will it be?
Federal Minister for Health and Aged Care Mark Butler said the RSV vaccine rollout has been modelled on the whooping cough vaccine in pregnant women, which is administered at around the same time and has an uptake rate of around 80%.
‘Maternal vaccination provides early protection for newborn children by reducing the risk of severe RSV disease in infants under 6 months of age by around 70%.'
The Department of Health and Aged Care
‘So we have good confidence that there will be a significant uptake of this maternal vaccine by pregnant Australian women,’ he added.
What is covered for pharmacists under the NIP?
According to the Department of Health and Aged Care, both the cost of the maternal RSV vaccine (Abrysvo) and the vaccine administration fee will be covered under the NIP and The National Immunisation Program Vaccinations in Pharmacy (NIPVIP) Program.
Abrysvo NIP vaccine stock will also be available to community pharmacists, said the spokesperson.
What about protection for neonates?
Access has also widened for more babies to receive a protection against RSV soon after birth, particularly those whose mother did not opt to have the vaccine during pregnancy.
Beyfortus (nirsevimab), an antibody therapy for the prevention of RSV-related lower respiratory tract disease, will be available in hospitals, immunisation clinics and general practices for infants before or during their first RSV season. Children up to 24 months of age who remain vulnerable to severe RSV disease throughout their second RSV season can also access the vaccine.
‘Beyfortus is a monoclonal antibody treatment which is administered to babies by injection,’ said Minister Butler. ‘[It can be received] immediately after birth … if their mother has not been vaccinated against RSV.’
Why did the government decide to take action against RSV?
Australia recorded the highest ever number of RSV cases this year, with 165,910 reported notifications.
Most cases were recorded in the 0–4 age cohort, among whom RSV can be fatal, and is the leading cause of hospitalisation for Australian children under five years of age.
The Australian Immunisation Foundation estimates that around 12,000 Australian babies aged 12 months or younger are admitted to hospital with RSV annually. Around 25% of these children will require intensive care.
The inclusion of an RSV vaccine in the NIP is an important step to protect newborn children and infants from severe RSV infection, said the spokesperson.
‘The highest rate of RSV-related hospitalisations is in infants during their first few months of life,’ said the spokesperson.
‘Infants with medical risk factors, such as being born very [premature], under 32 weeks gestational age, have an increased risk of severe disease.
‘Up to 80% of infants who are hospitalised due to RSV are otherwise healthy children with no predisposing conditions.’
What’s the expected impact?
The Immunisation Foundation of Australia has estimated that the nationwide availability of new RSV immunisations will help to keep 10,000 infants out of hospital with related bronchiolitis or pneumonia each year.
‘The immunisations being funded in Australia protect babies against severe RSV and have been shown to slash hospitalisation rates by up to 90 per cent,’ said Catherine Hughes AM, Founder and Director of the Immunisation Foundation of Australia.
Western Australia was the first state to implement an infant RSV immunisation program with Beyfortus. More than 23,000 infants received RSV protection this year, resulting in up to 84% fewer hospitalisations in immunised newborns compared to those who were not RSV protected. In Queensland, where a statewide infant RSV immunisation program commenced in April 2024, similar results were observed.
‘The exceptional results in Western Australia and Queensland contrast sharply with other parts of Australia where hospitals were overwhelmed by babies struggling to breathe due to severe RSV,’ she said.
Will older patients be able to receive the RSV vaccine under the NIP?
No. Well at least, not yet.
Vaccines can only be listed on the NIP after a positive recommendation from the Pharmaceutical Benefits Advisory Committee’s (PBAC) as required by the National Health Act 1953, said the spokesperson.
‘Several vaccine sponsors have made submissions in relation to RSV vaccines for older populations to the PBAC to consider for NIP listing,’ said the spokesperson.
‘The outcomes of these meetings will inform future government considerations regarding the potential listing of RSV vaccines on the NIP for older Australians.’
While a positive PBAC recommendation is an essential requirement in the NIP-listing process, other steps need to be completed before a vaccine can be given final approval for NIP listing, said the spokesperson.
‘These include negotiations with the relevant pharmaceutical company, finalisation of conditions for listing, quality and availability checks and final consideration by the government,’ said the spokesperson. ‘These considerations and decisions of government cannot be preempted.’
[post_title] => Government-funded RSV vaccines to protect infants from severe disease
[post_excerpt] => With cases of RSV spiking in 2024, the federal government announced free vaccination would be offered to eligible pregnant people and babies.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => government-funded-rsv-vaccines-to-protect-infants-from-severe-disease
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-13 13:26:32
[post_modified_gmt] => 2024-11-13 02:26:32
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28142
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Government-funded RSV vaccines to protect infants from severe disease
[title] => Government-funded RSV vaccines to protect infants from severe disease
[href] => https://www.australianpharmacist.com.au/government-funded-rsv-vaccines-to-protect-infants-from-severe-disease/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28146
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28134
[post_author] => 9164
[post_date] => 2024-11-11 12:48:48
[post_date_gmt] => 2024-11-11 01:48:48
[post_content] => Pharmacists and migrant community leaders, Sobia Hashmi MPS and Irfan Hashmi MPS, are the 2025 Local Heroes for South Australia, receiving their award on Saturday night in a ceremony in Adelaide.
The local heroes category of these Australia Day awards recognise role models who encourage others to be active in their own communities and become agents of positive change for a more diverse and inclusive Australia.
Over 20 years, Sobia and husband Irfan have transformed healthcare in remote and rural communities in South Australia. They’ve established six pharmacies in areas where there were previously none – which forced people to travel long distances for life-saving medicines and primary health care.
Sobia (48) and Irfan (51) are committed to serving their diverse communities. They employ staff who collectively speak 21 languages, allowing them to reach vulnerable populations and provide culturally sensitive healthcare. In 2020, they partnered with government to provide 24 free influenza vaccine clinics in outreach settings, providing 1200 vaccines to vulnerable people in South Australia.
Reflecting on the awards, Irfan and Sobia told Australian Pharmacist that the award was a celebration of the collective efforts of everyone who has been with them along the way, including their family, friends, colleagues, and the broader community.
‘To every individual who believed in us, who encouraged us to reach higher, and who shared in our vision of uplifting others, thank you. Your unwavering support drives us to do more, reach further, and connect deeper with those around us,’ they said.
Sobia and Irfan also reflected on the importance of community.
‘Together, we are stronger. Together, we make a difference. And together, let’s continue to build a healthier, more inclusive South Australia for all. This is just the beginning, and we are excited for the journey ahead,’ they said.
‘We are truly honoured and humbled to be named the 2025 Australian of the Year Award – Local Hero in SA recipients. This recognition strengthens our commitment to making a positive impact as pharmacists and community leaders, and it inspires us to continue serving the vibrant multicultural community that we call home.’
The couple have mentored countless intern pharmacists from overseas, coordinating multilingual education and outreach initiatives to help pharmacists enter the much-needed workforce in regional Australia. They host a free weekly webinar series, which has assisted 4,000 overseas pharmacists in passing their registration exams in the last 12 months alone.
Irfan previously was recognised as PSA’s 2009 South Australian Pharmacist of the Year.
[post_title] => Two pharmacists win state Australian of the Year 2025 award
[post_excerpt] => Sobia Hashmi MPS and Irfan Hashmi MPS will attend the Australian of the Year awards as finalists for the national local heroes title.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => two-pharmacists-win-state-australian-of-the-year-2025-award
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-13 13:26:46
[post_modified_gmt] => 2024-11-13 02:26:46
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28134
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Two pharmacists win state Australian of the Year 2025 award
[title] => Two pharmacists win state Australian of the Year 2025 award
[href] => https://www.australianpharmacist.com.au/two-pharmacists-win-state-australian-of-the-year-2025-award/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28140
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 27932
[post_author] => 235
[post_date] => 2024-11-07 00:53:00
[post_date_gmt] => 2024-11-06 13:53:00
[post_content] => A megatrend has begun in medicines. The increasingly large and full fridges found in pharmacies stand as a testament to the growing prevalence of injectable medicines – and are a sign of things to come.
In the near future, many daily tablets may be replaced with periodic appointments to have a medicine administered by injection.
The injectables are coming
Options for injectables and other non-oral dose forms such as patches, gels and sprays are rapidly growing, with these increasingly replacing medicinal therapies delivered through swallowing tablets, capsules or liquids. Pharmacists will recognise these examples.
Prolia (denosumab), which has been registered for the treatment of osteoporosis in Australia since 2010, offers a glimpse of the future, replacing daily or weekly tablets with biannual injections.1 Similarly, the relatively new cholesterol-lowering drug Leqvio (inclisiran) is administered every 6 months as a maintenance dose, after the initial induction doses, offering a new route for lipid modifying therapy.2
And Eli Lilly has a new US Food and Drug Administration-approved injectable, Kisunla (donanemab-azbt), coming out for the treatment of Alzheimer’s disease (AD).3 Delivered by infusion every 4 weeks, the drug works by targeting deposits of amyloid plaque in the brain, which is a key indicator of the presence of the debilitating, ultimately fatal brain disease.
Last month, one of the world leaders in AD research, Professor Colin Masters of The Florey Institute of Neuroscience and Mental Health in Melbourne, told neurologists and healthcare workers who treat patients with progressive neurodegenerative diseases of promising results from the Roche Dominant Inherited Alzheimer’s Network (DIAN) trial of the monoclonal antibody gantenerumab. Roche’s “Brain Shuttle” technology is now being used to cross the blood-brain barrier and then clear amyloid plaque aggregation with a newer generation, bio-specific, monoclonal antibody called trontinemab.
Prof Masters told a Creutzfeldt-Jakob Disease Support Group Network (CJDSGN)workshop on CJD and other prion diseases that early results from a trial of trontinemab are currently in pre-press in The Lancet.⁴

It’s also hoped, he says, that current intravenous AD drug models may evolve to be delivered subcutaneously via an autoinjector by patients at home.
Perhaps most revolutionary, however, are the advancements in HIV prevention. Recently, research into Gilead’s long-acting injection, lenacapavir (an agent for treatment of HIV), has shown promising results in pre-exposure prophylaxis (PrEP), and has been described as ‘the closest we have ever been to an HIV vaccine’ .⁵ At the AIDS 2024 conference in Germany in July, researchers presented their findings that twice-yearly lenacapavir demonstrated 100% efficacy for HIV prevention in cisgender women.⁶
‘The pace at which innovative, new medicines are entering the market is unprecedented,’ says Medicines Australia CEO Liz de Somer. ‘Advances in research, technology and innovation mean we can expect to see new forms of treatments – which include innovative new medicines and improved forms of existing medicines – becoming available.’
These are huge leaps forward in how health is treated, and pharmacists will need to adapt, says PSA National Board member Dr Shane Jackson FPS, community and credentialed pharmacist and lecturer in pharmacy at the University of Tasmania.
‘Medicines have always been an evolving space. Research on mRNA-delivered therapeutics has actually been around for about 20 years, and the pipeline of mRNA therapeutics is and will be a gamechanger in terms of treatment and prevention of disease in the future,’ he says.
‘What this means is that pharmacists will be needed more than ever because of their deep expertise in the use of medicines, and the term “medicines experts” will most likely evolve to “therapeutics experts”, noting the change from “medicine” to the complete management and prevention of disease.’
 New formats needed
New formats needed
One reason alternative delivery systems like injections and patches are becoming more prevalent is because they are critical for delivering new, biologically complex drugs.
As scientists have developed new treatments, they have created molecules that are too large or sensitive to be absorbed effectively through the digestive system. For example, Humira (adalimumab), the monoclonal antibody used to treat autoimmune conditions including juvenile arthritis and Crohn’s disease, is administered through subcutaneous injection because its large molecular structure would be ineffective if taken orally.⁷
Or take the testosterone transdermal delivery patch Androderm.8 Delivering testosterone directly through the skin provides a steady hormone level that can’t be achieved with oral testosterone.⁹
Technological advancements in mRNA technology, showcased in the production of COVID-19 vaccines, are also driving treatments and other preventive measures for different conditions.
‘Prior to the pandemic, mRNA-based drug products were focused primarily on treating oncology indications as opposed to infectious diseases, such as COVID-19,’ says Martin Gonzalez, Pfizer’s senior manager of product development.10
‘However, technical and scientific advancements have allowed researchers and drug developers to expand the use of mRNA to new therapeutic areas.’
For patients who inject themselves daily, there is also a growing preference for better ways to self-administer medicines. This focus on the patient has led to advances in medical devices in recent decades, introducing prefilled syringes, pens and automated electronic and infusion devices.

‘Much of the emphasis in contemporary drug design has shifted from just preserving basic quality attributes, such as safety, efficacy and potency, in a simple container,’ Mr Gonzalez says.10
‘Today’s [sterile injectable] drugs carry a more complex profile and incorporate new thinking about ways of preserving the value of the drug while also providing additional benefits, including precise, easy-to-administer delivery systems for better dose compliance.’
Improving medicine adherence
According to the World Health Organization, around 50% of patients with chronic illnesses in developed countries don’t take their medicines as prescribed.11
The rates are even lower in developing nations. There are myriad reasons for poor medicine adherence, including low health literacy, the prescription of complex drug regimens and limited access to care.12
Long-acting therapies may also be beneficial for hard-to-reach populations, such as those experiencing homelessness or substance use problems. And in the case of those living with HIV, long-acting drugs might also be useful for children, says Dr Charles Flexner, HIV expert at Johns Hopkins University. Globally, just 50% of children diagnosed with HIV are receiving treatment, in part due to a lack of drug versions made for children.13
‘With long-acting formulations, that will no longer be the case,’ Dr Flexner says.13 ‘Children will be able to use the same formulation as adults, just at a different dose.’
Breakthrough in injectable PrEPLong-acting injectables for HIV treatment and prevention are providing convenience, promoting better adherence, and helping to reduce the stigma and discrimination that might come with taking a daily pill.14 In Australia, there is currently one injectable HIV medicine listed on the Pharmaceutical Benefits Scheme (PBS) – Cabenuva (cabotegravir/rilpivirine), which requires injections every 2 months.15 Cabotegravir-LA for pre-exposure prophylaxis (PrEP) has been approved by the Therapeutic Goods Administration (TGA) but is not yet listed on the PBS,16 and lenacapavir is also TGA-approved but not PBS listed for treating multidrug-resistant HIV in combination with other antiretroviral therapy. Globally, 6-monthly injections of lenacapavir have also been trialled for PrEP, with extraordinary results. Clinical trial data released this year in a study of cisgender men, transgender men, transgender women, and nonbinary individuals who have sex with partners assigned male at birth showed that using lenacapavir results in a 96% lower HIV rate compared with the expected incidence of infection, and an 89% lower HIV rate compared with oral PrEP.17
Trials have also shown an efficacy rate of 100% among cisgender women in South Africa and Uganda.
Professor Sharon Lewin, Director of the Peter Doherty Institute for Infection and Immunity at the University of Melbourne, and immediate past president of the International AIDS Society, described the results as ‘a breakthrough advance with huge public health potential’.
‘If approved and delivered – rapidly, affordably and equitably – to those who need or want it, this long-acting tool could help accelerate global progress in HIV prevention,’ Professor Lewin said.⁶
When it comes to long-acting injectables for HIV treatment and prevention: watch this space. Clinical trial data released this year in a study of cisgender men, transgender men, transgender women, and nonbinary individuals who have sex with partners assigned male at birth showed that using lenacapavir results in a 96% lower HIV rate compared with the expected incidence of infection, and an 89% lower HIV rate compared with oral PrEP.17
Trials have also shown an efficacy rate of 100% among cisgender women in South Africa and Uganda.
Professor Sharon Lewin, Director of the Peter Doherty Institute for Infection and Immunity at the University of Melbourne, and immediate past president of the International AIDS Society, described the results as ‘a breakthrough advance with huge public health potential’.
‘If approved and delivered – rapidly, affordably and equitably – to those who need or want it, this long-acting tool could help accelerate global progress in HIV prevention,’ Professor Lewin said.⁶
When it comes to long-acting injectables for HIV treatment and prevention: watch this space. |
As more injectable medicines come onto the market, the pharmacy of the near future will need more consultation rooms and more dispensary refrigerator space.
Pharmacy practice will likely involve more direct patient care, including administering injections and managing complex treatment regimens. Those who fail to adapt, for example by not learning to inject safely, risk becoming obsolete, as the profession increasingly shifts to a more hands-on role.
‘In terms of medicines administration [by injection], this is a newish activity that pharmacists are undertaking,’ Dr Jackson points out. ‘It is becoming increasingly relevant because of a lack of access to general practice care and the acknowledgement that this activity is and has always been within the scope of practice of a pharmacist in terms of education and training.
‘Pharmacists need to ensure they are competent in terms of their training (vaccination certified, medicines administration training has been completed) and that they inform themselves of the relevant information related to each drug being administered.
 ‘In my view, it’s analogous to dispensing a new drug that you haven’t come across before. You understand the relevant information related to the drug from a safety and effectiveness point of view, you communicate with the patient regarding relevant counselling points, and you document relevant information.’
‘In my view, it’s analogous to dispensing a new drug that you haven’t come across before. You understand the relevant information related to the drug from a safety and effectiveness point of view, you communicate with the patient regarding relevant counselling points, and you document relevant information.’
But the future isn’t just about the administration of a medicine. Rather, Dr Jackson says, this is just the start of pharmacists ‘being more involved and taking more responsibility and accountability for patient care’.
‘Regulatory misunderstanding and regulatory impediments have for a long time prevented pharmacists from doing more in the prescribing, administration and review of medicines.
‘We are seeing these barriers being reduced, albeit slowly in some jurisdictions, to allow pharmacists to do more, to practise to their full scope in terms of medicines management.
‘Ideally, pharmacists should be empowering patients to better take control of their own health care. For most of the medicines we see currently, patients with appropriate support can self-administer,’ says Dr Jackson.
‘In some cases, there may be barriers in place and pharmacists may deliver regular injections for these patients. It’s a case-by-case basis with the patient at the centre of care.’
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28084
[post_author] => 3410
[post_date] => 2024-11-06 15:56:15
[post_date_gmt] => 2024-11-06 04:56:15
[post_content] => After months of anticipation, the Unleashing the potential of our health workforce – Scope of practice review was released yesterday (5 November) – with many of the key recommendations echoing the long-held concerns of the PSA and pharmacists across Australia.
Australian Pharmacist has rounded up some of the key takeouts from the report.
Pharmacists are leaving the profession at an alarming rate
Pharmacy has a high attrition rate compared with other healthcare professions. Among 19 healthcare professions, pharmacy had the fifth highest exit rate of 8.7% in 2023 – almost double that of medical professionals (4.7%).
The professions with the highest exit rates are those that face significant barriers to working to their full scope of practice, the review found.
While there are several factors that impact exit rates, allowing pharmacists to work to their full scope of practice is a crucial factor for strengthening the profession’s retention rate – improving recognition for professional skills, capability and contribution to enhance continuity of care.
‘This report really makes clear that there are all sorts of artificial, inefficient restrictions on what nurses, pharmacists, GPs, and other health professionals are allowed to do that bears no relationship to their training,’ said federal Minister for Health and Aged Care Mark Butler.
Inconsistencies in vaccine schedules for pharmacists are ‘needless’
Pharmacist vaccinators are trained in accordance with the National Immunisation Education Framework, ensuring high standards in vaccine administration and competence.
But the report found that the difference in state and territory laws dictating which vaccines can be administered by pharmacists has led to disparities in access – not only causing confusion among patients but leading to significant inefficiencies.
Legislative differences between states and territories also means that a vaccine subsidised in one region might not be covered in another.
Harmonising these regulations by reviewing Drugs and Poisons Acts would promote equitable vaccine access nationwide, allowing pharmacists’ to provide consistent healthcare services regardless of location.
Aligning funding arrangements for vaccination is also crucial, the review found. While the National Immunisation Program Vaccinations in Pharmacy (NIPVIP) provides government funding for certain vaccines, access to others depends on a mix of user-pay systems and varying jurisdictional funding – creating inconsistencies in affordability and accessibility across states and territories.
Standardising funding mechanisms would ensure subsidies are uniformly applied – making vaccinations more affordable and accessible to all Australians.
It will take some time to implement change, but there are some steps governments and regulators can take now
While some of the recommendations in the review, such as harmonising vaccination legislation, can be achieved in a timely fashion, others are sweeping reforms that will take many years, such as restructuring healthcare education – which currently impacts students and qualified pharmacists’ ability to work to their full scope.
The review recommended the Commonwealth establish a primary care workforce development program to support the development and retention of a skilled, stable, and collaborative primary care workforce through enhanced curriculum, training, placement, and career development opportunities for students, supervisors, mentors, and health professionals.
The current funding model must be overhauled
The current fee-for-service arrangement in primary care incentivises high-turnover care – with payments to providers based on the number and type of care episodes delivered.
This model limits the ability of health professionals to work to their full scope and reduces multidisciplinary collaboration – with some healthcare professionals funded for certain services while others are not, including lack of funding for pharmacists to participate in multidisciplinary case conferences.
To address this, the review recommends introducing a blended payment model to complement the fee-for-service system. This model would enable access to multidisciplinary healthcare delivered by professionals working to their full scope of practice in primary care.
An independent mechanism would be established to advise on pricing and payment levels for the blended payment, ensuring adjustments based on the risk profile of patient populations.
But it’s unlikely to be a quick fix. The review suggests the model would need to be implemented progressively over a 7-year period, beginning with priority areas such as rural and remote regions, Aboriginal Community Controlled Health Organisations, and underserviced regional and outer metropolitan areas.
Pharmacist prescribing programs should be nationally consistent
Implementing pharmacists prescribing rights has been an unnecessarily complex and prolonged process, with ad-hoc investigations, one-off reviews, and small-scale pilots.
Adopting an activity-based approach would streamline regulation for community pharmacists in prescribing medications and promote consistency across jurisdictions.
Introducing a dedicated mechanism to assess health workforce models would also fill a crucial gap, facilitating the systematic adoption of multidisciplinary primary care models that include pharmacists much like the successful models implemented in the United Kingdom.
Improved use of technology should form the backbone of scope of practice changes
A key theme in the review was the need for better use of technology across the board to expand scopes of practice and efficiencies, improving quality of care.
Potential areas for reform identified by the review include establishing access to real‑time patient information, introducing platforms for secure messaging and digital referrals and mandating participation in a multidisciplinary care team for primary care providers.
‘[We need to] improve the digital capability of a system that still uses far too many fax machines and too much paper,’ said Minister Butler.
The government will respond, in time
The government is yet to respond to the key recommendations in the report, with Minister Butler confirming he will not ‘respond to each of the ideas’.
‘We want to consider them, but a lot of them do have a lot of common sense,’ he said.
Other key stakeholders will also need to be consulted.
‘Many of the recommendations will require collaboration between the Commonwealth and state and territory governments, as well as consultation with peak professional organisations, AHPRA, patient groups, and the sector more broadly. I look forward to these discussions,’ Minister Butler added.
But PSA has called for the government to accept all 18 recommendations and put forward a plan of action now.
This review confirms PSA’s view that inconsistent regulations, unnecessary restrictions on practice, and siloed workforces are having a negative impact on patient access to quality health care, said PSA National President Associate Professor Fei Sim.
‘This report recognises the core role of pharmacies and pharmacists as primary healthcare providers and recommends a multidisciplinary approach to patient care,’ she said.
‘There is a clear alignment between Cormack’s recommendations and the actions in PSA’s vision for the pharmacy profession, Pharmacists in 2030. Both present a clear vision for the future that requires collaboration for a health system that works for patients.’
What the health sector is saying
The Australian Medical Association has said that the government ‘must resist’ changes to scope of practice, maintaining its position for even more investment into general practice.
Meanwhile, the Royal Australian College of GPs said the recommendations, if implemented, would ‘raid Medicare’, setting up for a ‘two-tiered health system where those who can afford to see a GP will, and those who can’t, don’t.’
But the Australian Nursing and Midwifery Federation said the review allows highly-trained health professionals to best utilise their skills, education and experience, allowing for the delivery of integrated, quality healthcare services across the community.
Support also came from the National Rural Health Alliance, who welcomed the recommendations that seek to address some of the ‘inequalities faced by rural Australians when it comes to accessing healthcare.’
Outside of the health sector, the Business Council of Australia also welcomed the report, citing improving ‘productivity, patient experience and workforce satisfaction’ as necessary to a sustainable health system.
[post_title] => Key recommendations to strengthen pharmacists’ role in healthcare
[post_excerpt] => The scope of practice review recommends sweeping legislative change and solutions to funding challenges to improve healthcare services.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => key-recommendation-to-strengthen-pharmacists-role-in-healthcare
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-06 17:01:11
[post_modified_gmt] => 2024-11-06 06:01:11
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28084
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Key recommendations to strengthen pharmacists’ role in healthcare
[title] => Key recommendations to strengthen pharmacists’ role in healthcare
[href] => https://www.australianpharmacist.com.au/key-recommendation-to-strengthen-pharmacists-role-in-healthcare/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28086
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28164
[post_author] => 3410
[post_date] => 2024-11-13 12:50:58
[post_date_gmt] => 2024-11-13 01:50:58
[post_content] => The Therapeutic Goods Administration (TGA) has worked with Phenergan manufacturer Sanofi to develop a new contraindication for the medicine in children under 6.
The decision to restrict use of the medicine in this age cohort – commonly used to treat allergies, travel sickness and nausea – is based on a thorough evaluation of new scientific evidence that the risks outweigh the benefits, a spokesperson for Sanofi told Australian Pharmacist.
‘Following recent evaluations made by Sanofi Consumer Healthcare Pty Ltd, including a benefit-risk assessment, the research has shown a causal association between promethazine and safety concerns,’ said this spokesperson.
The sponsor-initiated update was prompted by advice from the TGA Advisory Committee on Medicines (ACM) – first-generation oral sedating antihistamines – do not use in children, said a spokesperson from the TGA.
‘Further review by the sponsor of cumulative safety data in children 2 to 5 years of age demonstrated sufficient evidence of a causal association between promethazine and psychiatric and central nervous system adverse events in this age group,’ the TGA spokesperson told AP.
The contraindication comes after Medsafe, the New Zealand Medicines and Medical Devices Safety Authority, moved to contraindicate the use of the medicine in children under 6 due to the potential for fatal respiratory depression, psychiatric and central nervous system (CNS) events.
AP understands that the contraindication will affect other products. A spokesperson for AFT said a variation has been submitted to update the product information and label on Allersoothe Elixir with a change to the age indication from children 2 years and older to children 6 years and older. This submission is pending approval.
Will the packaging change?
Not immediately.
New labels for promethazine-containing products will be rolled out in 2025 due to production and logistics lead times, said the Sanofi spokesperson.
‘No immediate action is required regarding current stock. There is no need to set aside existing medications, as this communication does not constitute a recall,’ said the spokesperson. ‘Similarly, the revised labels do not create any changes in the ordering process.
The product information for Phenergan has been updated and is available here.
What should pharmacists do if they get a Phenergan script for an 18 month old infant?
The use of promethazine in children under 6 years of age is now both contraindicated and off label, said Peter Guthrey MPS, PSA Senior Pharmacist – strategic policy.
‘This means that if you choose to dispense, both the prescriber and dispenser carry the full indemnity risk, and you need to get the patient to provide informed consent,’ he said.
Should a parent present with a script for promethazine for use in a child under 6 years of age, pharmacists should contact the prescriber to discuss the risks and benefits, noting that it's contraindicated.
Is there any situation where it would be appropriate to dispense Phenergan to a young child?
It would need to be a pretty compelling case, where the benefit to a child outweighed the risk of respiratory depression, psychiatric or CNS events , said Mr Guthrey.
‘Given it’s a documented contraindication, it'd be pretty hard to demonstrate the medicine is ‘‘safe and therapeutically appropriate’’,’ he said.
‘It is going to be difficult to find a situation where supply is clinically justified and pharmacists have met their obligations to patient safety.’
What about prescribing Phenergan as a Schedule 3 medicine?
If a parent requests promethazine as a Schedule 3 medicine for someone under the age of 6 years, generally alternate products or advice for treatment should be provided following a discussion.
‘While a pharmacist prescribing promethazine as a Pharmacist Only Medicine is lawful for children aged 2-5 years, it is still contraindicated,’ said Mr Guthrey. ‘There would be very few, if any, situations where prescribing the medicine where contraindicated would be warranted.’
What about phenylephrine?
There are some combination phenylephrine products indicated for children under 6 years of age for nasal congestion. However, there is plenty of evidence showing that oral phenylephrine products are ineffective as a nasal decongestant.
In fact, the United States Food and Drug Administration (FDA) recently announced it will move to ban oral phenylephrine products because they simply don't work.
‘Based on our review of available data, and consistent with the advice of the advisory committee, we are taking this next step in the process to propose removing oral phenylephrine because it is not effective as a nasal decongestant,’ said Patrizia Cavazzoni, M.D., director of the FDA’s Center for Drug Evaluation and Research .
While a spokesperson for the TGA told Australian Pharmacist back in July that there are ‘no plans’ to review the effectiveness of oral phenylephrine, it will continue to monitor the outcomes of the FDA review.
What advice should pharmacists provide?
For children with allergies, non-sedating histamines are first line.
The best thing parents can do when a child under 6 years of age has cough or cold symptoms is to wait it out, with a review by a medical practitioner when appropriate.
‘It's about reassurance to parents that the cough in itself isn't harmful, and that kids don’t always need medicines for a cold – they need time and supportive therapy,’ said Mr Guthrey.
It’s important that pharmacists give parents confidence that they're doing the right thing by not treating the cough, and providing symptomatic relief for fever and chills, and ensuring they are appropriately counselled on when review by a medical practitioner may be appropriate.
For more information, refer to the Australian Pharmaceutical Formulary and Handbook treatment guidelines on:
[post_title] => Do not supply Phenergan to children under 6, manufacturer warns
[post_excerpt] => The TGA has worked with Phenergan manufacturer Sanofi to develop a new contraindication for the medicine in children under 6.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => do-not-supply-phenergan-to-children-under-6-manufacturer-warns
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-13 16:15:31
[post_modified_gmt] => 2024-11-13 05:15:31
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28164
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Do not supply Phenergan to children under 6, manufacturer warns
[title] => Do not supply Phenergan to children under 6, manufacturer warns
[href] => https://www.australianpharmacist.com.au/do-not-supply-phenergan-to-children-under-6-manufacturer-warns/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28167
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28142
[post_author] => 3410
[post_date] => 2024-11-11 15:55:46
[post_date_gmt] => 2024-11-11 04:55:46
[post_content] => With cases of Respiratory syncytial virus (RSV) spiking this year, the federal government announced yesterday (10 November) that free vaccination would be offered to eligible pregnant people and babies.
Before the 2025 winter season, the RSV vaccine will be available under the National Immunisation Program (NIP) for all people in the third trimester of pregnancy via the Australian Infant RSV Immunisation Program.
Which RSV vaccines will pharmacists administer?
The RSV immunisation program will offer two Therapeutic Goods Administration approved protections against severe RSV.
Pharmacists can administer the maternal vaccine, Abrysvo, to pregnant women between 28-36 weeks of gestation.
Maternal vaccination provides early protection for newborn children by reducing the risk of severe RSV disease in infants under 6 months of age by around 70%, a spokesperson from the Department of Health and Aged Care told Australian Pharmacist.
‘This is [through] passive protection by transplacental transfer of RSV-specific antibodies from the mother to the foetus during pregnancy.’
How popular will it be?
Federal Minister for Health and Aged Care Mark Butler said the RSV vaccine rollout has been modelled on the whooping cough vaccine in pregnant women, which is administered at around the same time and has an uptake rate of around 80%.
‘Maternal vaccination provides early protection for newborn children by reducing the risk of severe RSV disease in infants under 6 months of age by around 70%.'
The Department of Health and Aged Care
‘So we have good confidence that there will be a significant uptake of this maternal vaccine by pregnant Australian women,’ he added.
What is covered for pharmacists under the NIP?
According to the Department of Health and Aged Care, both the cost of the maternal RSV vaccine (Abrysvo) and the vaccine administration fee will be covered under the NIP and The National Immunisation Program Vaccinations in Pharmacy (NIPVIP) Program.
Abrysvo NIP vaccine stock will also be available to community pharmacists, said the spokesperson.
What about protection for neonates?
Access has also widened for more babies to receive a protection against RSV soon after birth, particularly those whose mother did not opt to have the vaccine during pregnancy.
Beyfortus (nirsevimab), an antibody therapy for the prevention of RSV-related lower respiratory tract disease, will be available in hospitals, immunisation clinics and general practices for infants before or during their first RSV season. Children up to 24 months of age who remain vulnerable to severe RSV disease throughout their second RSV season can also access the vaccine.
‘Beyfortus is a monoclonal antibody treatment which is administered to babies by injection,’ said Minister Butler. ‘[It can be received] immediately after birth … if their mother has not been vaccinated against RSV.’
Why did the government decide to take action against RSV?
Australia recorded the highest ever number of RSV cases this year, with 165,910 reported notifications.
Most cases were recorded in the 0–4 age cohort, among whom RSV can be fatal, and is the leading cause of hospitalisation for Australian children under five years of age.
The Australian Immunisation Foundation estimates that around 12,000 Australian babies aged 12 months or younger are admitted to hospital with RSV annually. Around 25% of these children will require intensive care.
The inclusion of an RSV vaccine in the NIP is an important step to protect newborn children and infants from severe RSV infection, said the spokesperson.
‘The highest rate of RSV-related hospitalisations is in infants during their first few months of life,’ said the spokesperson.
‘Infants with medical risk factors, such as being born very [premature], under 32 weeks gestational age, have an increased risk of severe disease.
‘Up to 80% of infants who are hospitalised due to RSV are otherwise healthy children with no predisposing conditions.’
What’s the expected impact?
The Immunisation Foundation of Australia has estimated that the nationwide availability of new RSV immunisations will help to keep 10,000 infants out of hospital with related bronchiolitis or pneumonia each year.
‘The immunisations being funded in Australia protect babies against severe RSV and have been shown to slash hospitalisation rates by up to 90 per cent,’ said Catherine Hughes AM, Founder and Director of the Immunisation Foundation of Australia.
Western Australia was the first state to implement an infant RSV immunisation program with Beyfortus. More than 23,000 infants received RSV protection this year, resulting in up to 84% fewer hospitalisations in immunised newborns compared to those who were not RSV protected. In Queensland, where a statewide infant RSV immunisation program commenced in April 2024, similar results were observed.
‘The exceptional results in Western Australia and Queensland contrast sharply with other parts of Australia where hospitals were overwhelmed by babies struggling to breathe due to severe RSV,’ she said.
Will older patients be able to receive the RSV vaccine under the NIP?
No. Well at least, not yet.
Vaccines can only be listed on the NIP after a positive recommendation from the Pharmaceutical Benefits Advisory Committee’s (PBAC) as required by the National Health Act 1953, said the spokesperson.
‘Several vaccine sponsors have made submissions in relation to RSV vaccines for older populations to the PBAC to consider for NIP listing,’ said the spokesperson.
‘The outcomes of these meetings will inform future government considerations regarding the potential listing of RSV vaccines on the NIP for older Australians.’
While a positive PBAC recommendation is an essential requirement in the NIP-listing process, other steps need to be completed before a vaccine can be given final approval for NIP listing, said the spokesperson.
‘These include negotiations with the relevant pharmaceutical company, finalisation of conditions for listing, quality and availability checks and final consideration by the government,’ said the spokesperson. ‘These considerations and decisions of government cannot be preempted.’
[post_title] => Government-funded RSV vaccines to protect infants from severe disease
[post_excerpt] => With cases of RSV spiking in 2024, the federal government announced free vaccination would be offered to eligible pregnant people and babies.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => government-funded-rsv-vaccines-to-protect-infants-from-severe-disease
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-13 13:26:32
[post_modified_gmt] => 2024-11-13 02:26:32
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28142
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Government-funded RSV vaccines to protect infants from severe disease
[title] => Government-funded RSV vaccines to protect infants from severe disease
[href] => https://www.australianpharmacist.com.au/government-funded-rsv-vaccines-to-protect-infants-from-severe-disease/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28146
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28134
[post_author] => 9164
[post_date] => 2024-11-11 12:48:48
[post_date_gmt] => 2024-11-11 01:48:48
[post_content] => Pharmacists and migrant community leaders, Sobia Hashmi MPS and Irfan Hashmi MPS, are the 2025 Local Heroes for South Australia, receiving their award on Saturday night in a ceremony in Adelaide.
The local heroes category of these Australia Day awards recognise role models who encourage others to be active in their own communities and become agents of positive change for a more diverse and inclusive Australia.
Over 20 years, Sobia and husband Irfan have transformed healthcare in remote and rural communities in South Australia. They’ve established six pharmacies in areas where there were previously none – which forced people to travel long distances for life-saving medicines and primary health care.
Sobia (48) and Irfan (51) are committed to serving their diverse communities. They employ staff who collectively speak 21 languages, allowing them to reach vulnerable populations and provide culturally sensitive healthcare. In 2020, they partnered with government to provide 24 free influenza vaccine clinics in outreach settings, providing 1200 vaccines to vulnerable people in South Australia.
Reflecting on the awards, Irfan and Sobia told Australian Pharmacist that the award was a celebration of the collective efforts of everyone who has been with them along the way, including their family, friends, colleagues, and the broader community.
‘To every individual who believed in us, who encouraged us to reach higher, and who shared in our vision of uplifting others, thank you. Your unwavering support drives us to do more, reach further, and connect deeper with those around us,’ they said.
Sobia and Irfan also reflected on the importance of community.
‘Together, we are stronger. Together, we make a difference. And together, let’s continue to build a healthier, more inclusive South Australia for all. This is just the beginning, and we are excited for the journey ahead,’ they said.
‘We are truly honoured and humbled to be named the 2025 Australian of the Year Award – Local Hero in SA recipients. This recognition strengthens our commitment to making a positive impact as pharmacists and community leaders, and it inspires us to continue serving the vibrant multicultural community that we call home.’
The couple have mentored countless intern pharmacists from overseas, coordinating multilingual education and outreach initiatives to help pharmacists enter the much-needed workforce in regional Australia. They host a free weekly webinar series, which has assisted 4,000 overseas pharmacists in passing their registration exams in the last 12 months alone.
Irfan previously was recognised as PSA’s 2009 South Australian Pharmacist of the Year.
[post_title] => Two pharmacists win state Australian of the Year 2025 award
[post_excerpt] => Sobia Hashmi MPS and Irfan Hashmi MPS will attend the Australian of the Year awards as finalists for the national local heroes title.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => two-pharmacists-win-state-australian-of-the-year-2025-award
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-13 13:26:46
[post_modified_gmt] => 2024-11-13 02:26:46
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28134
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Two pharmacists win state Australian of the Year 2025 award
[title] => Two pharmacists win state Australian of the Year 2025 award
[href] => https://www.australianpharmacist.com.au/two-pharmacists-win-state-australian-of-the-year-2025-award/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28140
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 27932
[post_author] => 235
[post_date] => 2024-11-07 00:53:00
[post_date_gmt] => 2024-11-06 13:53:00
[post_content] => A megatrend has begun in medicines. The increasingly large and full fridges found in pharmacies stand as a testament to the growing prevalence of injectable medicines – and are a sign of things to come.
In the near future, many daily tablets may be replaced with periodic appointments to have a medicine administered by injection.
The injectables are coming
Options for injectables and other non-oral dose forms such as patches, gels and sprays are rapidly growing, with these increasingly replacing medicinal therapies delivered through swallowing tablets, capsules or liquids. Pharmacists will recognise these examples.
Prolia (denosumab), which has been registered for the treatment of osteoporosis in Australia since 2010, offers a glimpse of the future, replacing daily or weekly tablets with biannual injections.1 Similarly, the relatively new cholesterol-lowering drug Leqvio (inclisiran) is administered every 6 months as a maintenance dose, after the initial induction doses, offering a new route for lipid modifying therapy.2
And Eli Lilly has a new US Food and Drug Administration-approved injectable, Kisunla (donanemab-azbt), coming out for the treatment of Alzheimer’s disease (AD).3 Delivered by infusion every 4 weeks, the drug works by targeting deposits of amyloid plaque in the brain, which is a key indicator of the presence of the debilitating, ultimately fatal brain disease.
Last month, one of the world leaders in AD research, Professor Colin Masters of The Florey Institute of Neuroscience and Mental Health in Melbourne, told neurologists and healthcare workers who treat patients with progressive neurodegenerative diseases of promising results from the Roche Dominant Inherited Alzheimer’s Network (DIAN) trial of the monoclonal antibody gantenerumab. Roche’s “Brain Shuttle” technology is now being used to cross the blood-brain barrier and then clear amyloid plaque aggregation with a newer generation, bio-specific, monoclonal antibody called trontinemab.
Prof Masters told a Creutzfeldt-Jakob Disease Support Group Network (CJDSGN)workshop on CJD and other prion diseases that early results from a trial of trontinemab are currently in pre-press in The Lancet.⁴

It’s also hoped, he says, that current intravenous AD drug models may evolve to be delivered subcutaneously via an autoinjector by patients at home.
Perhaps most revolutionary, however, are the advancements in HIV prevention. Recently, research into Gilead’s long-acting injection, lenacapavir (an agent for treatment of HIV), has shown promising results in pre-exposure prophylaxis (PrEP), and has been described as ‘the closest we have ever been to an HIV vaccine’ .⁵ At the AIDS 2024 conference in Germany in July, researchers presented their findings that twice-yearly lenacapavir demonstrated 100% efficacy for HIV prevention in cisgender women.⁶
‘The pace at which innovative, new medicines are entering the market is unprecedented,’ says Medicines Australia CEO Liz de Somer. ‘Advances in research, technology and innovation mean we can expect to see new forms of treatments – which include innovative new medicines and improved forms of existing medicines – becoming available.’
These are huge leaps forward in how health is treated, and pharmacists will need to adapt, says PSA National Board member Dr Shane Jackson FPS, community and credentialed pharmacist and lecturer in pharmacy at the University of Tasmania.
‘Medicines have always been an evolving space. Research on mRNA-delivered therapeutics has actually been around for about 20 years, and the pipeline of mRNA therapeutics is and will be a gamechanger in terms of treatment and prevention of disease in the future,’ he says.
‘What this means is that pharmacists will be needed more than ever because of their deep expertise in the use of medicines, and the term “medicines experts” will most likely evolve to “therapeutics experts”, noting the change from “medicine” to the complete management and prevention of disease.’
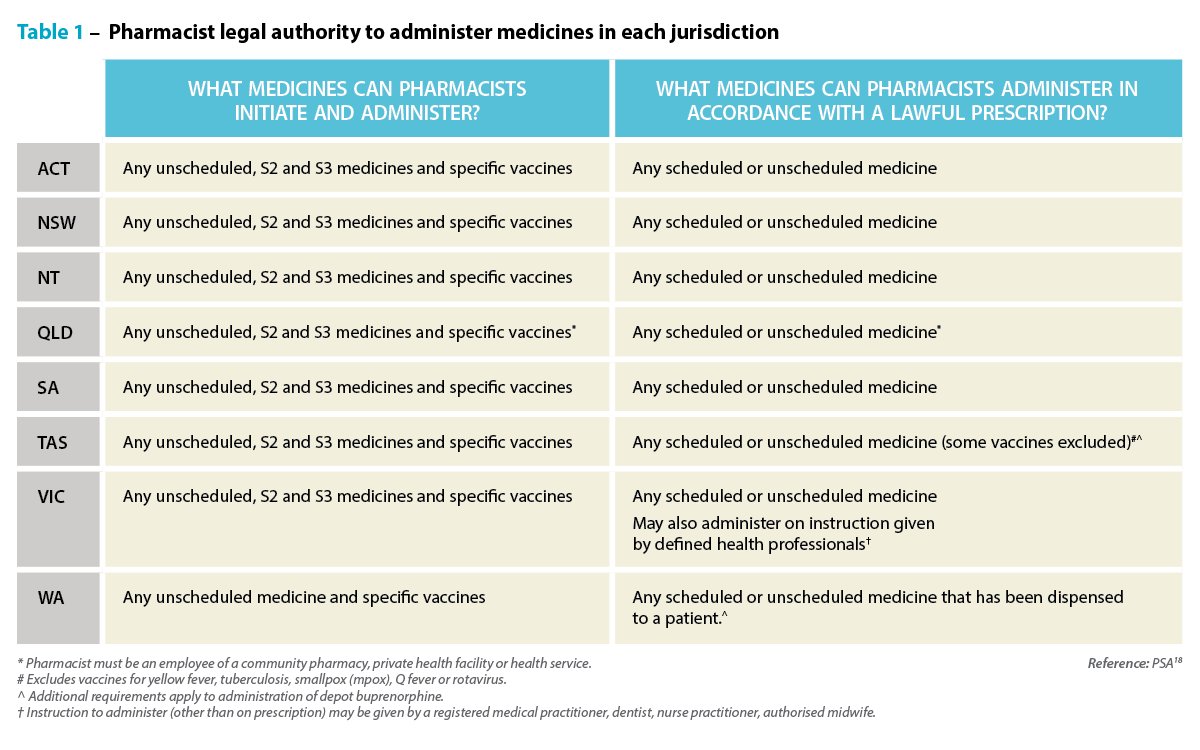 New formats needed
New formats needed
One reason alternative delivery systems like injections and patches are becoming more prevalent is because they are critical for delivering new, biologically complex drugs.
As scientists have developed new treatments, they have created molecules that are too large or sensitive to be absorbed effectively through the digestive system. For example, Humira (adalimumab), the monoclonal antibody used to treat autoimmune conditions including juvenile arthritis and Crohn’s disease, is administered through subcutaneous injection because its large molecular structure would be ineffective if taken orally.⁷
Or take the testosterone transdermal delivery patch Androderm.8 Delivering testosterone directly through the skin provides a steady hormone level that can’t be achieved with oral testosterone.⁹
Technological advancements in mRNA technology, showcased in the production of COVID-19 vaccines, are also driving treatments and other preventive measures for different conditions.
‘Prior to the pandemic, mRNA-based drug products were focused primarily on treating oncology indications as opposed to infectious diseases, such as COVID-19,’ says Martin Gonzalez, Pfizer’s senior manager of product development.10
‘However, technical and scientific advancements have allowed researchers and drug developers to expand the use of mRNA to new therapeutic areas.’
For patients who inject themselves daily, there is also a growing preference for better ways to self-administer medicines. This focus on the patient has led to advances in medical devices in recent decades, introducing prefilled syringes, pens and automated electronic and infusion devices.

‘Much of the emphasis in contemporary drug design has shifted from just preserving basic quality attributes, such as safety, efficacy and potency, in a simple container,’ Mr Gonzalez says.10
‘Today’s [sterile injectable] drugs carry a more complex profile and incorporate new thinking about ways of preserving the value of the drug while also providing additional benefits, including precise, easy-to-administer delivery systems for better dose compliance.’
Improving medicine adherence
According to the World Health Organization, around 50% of patients with chronic illnesses in developed countries don’t take their medicines as prescribed.11
The rates are even lower in developing nations. There are myriad reasons for poor medicine adherence, including low health literacy, the prescription of complex drug regimens and limited access to care.12
Long-acting therapies may also be beneficial for hard-to-reach populations, such as those experiencing homelessness or substance use problems. And in the case of those living with HIV, long-acting drugs might also be useful for children, says Dr Charles Flexner, HIV expert at Johns Hopkins University. Globally, just 50% of children diagnosed with HIV are receiving treatment, in part due to a lack of drug versions made for children.13
‘With long-acting formulations, that will no longer be the case,’ Dr Flexner says.13 ‘Children will be able to use the same formulation as adults, just at a different dose.’
Breakthrough in injectable PrEPLong-acting injectables for HIV treatment and prevention are providing convenience, promoting better adherence, and helping to reduce the stigma and discrimination that might come with taking a daily pill.14 In Australia, there is currently one injectable HIV medicine listed on the Pharmaceutical Benefits Scheme (PBS) – Cabenuva (cabotegravir/rilpivirine), which requires injections every 2 months.15 Cabotegravir-LA for pre-exposure prophylaxis (PrEP) has been approved by the Therapeutic Goods Administration (TGA) but is not yet listed on the PBS,16 and lenacapavir is also TGA-approved but not PBS listed for treating multidrug-resistant HIV in combination with other antiretroviral therapy. Globally, 6-monthly injections of lenacapavir have also been trialled for PrEP, with extraordinary results. Clinical trial data released this year in a study of cisgender men, transgender men, transgender women, and nonbinary individuals who have sex with partners assigned male at birth showed that using lenacapavir results in a 96% lower HIV rate compared with the expected incidence of infection, and an 89% lower HIV rate compared with oral PrEP.17
Trials have also shown an efficacy rate of 100% among cisgender women in South Africa and Uganda.
Professor Sharon Lewin, Director of the Peter Doherty Institute for Infection and Immunity at the University of Melbourne, and immediate past president of the International AIDS Society, described the results as ‘a breakthrough advance with huge public health potential’.
‘If approved and delivered – rapidly, affordably and equitably – to those who need or want it, this long-acting tool could help accelerate global progress in HIV prevention,’ Professor Lewin said.⁶
When it comes to long-acting injectables for HIV treatment and prevention: watch this space. Clinical trial data released this year in a study of cisgender men, transgender men, transgender women, and nonbinary individuals who have sex with partners assigned male at birth showed that using lenacapavir results in a 96% lower HIV rate compared with the expected incidence of infection, and an 89% lower HIV rate compared with oral PrEP.17
Trials have also shown an efficacy rate of 100% among cisgender women in South Africa and Uganda.
Professor Sharon Lewin, Director of the Peter Doherty Institute for Infection and Immunity at the University of Melbourne, and immediate past president of the International AIDS Society, described the results as ‘a breakthrough advance with huge public health potential’.
‘If approved and delivered – rapidly, affordably and equitably – to those who need or want it, this long-acting tool could help accelerate global progress in HIV prevention,’ Professor Lewin said.⁶
When it comes to long-acting injectables for HIV treatment and prevention: watch this space. |
As more injectable medicines come onto the market, the pharmacy of the near future will need more consultation rooms and more dispensary refrigerator space.
Pharmacy practice will likely involve more direct patient care, including administering injections and managing complex treatment regimens. Those who fail to adapt, for example by not learning to inject safely, risk becoming obsolete, as the profession increasingly shifts to a more hands-on role.
‘In terms of medicines administration [by injection], this is a newish activity that pharmacists are undertaking,’ Dr Jackson points out. ‘It is becoming increasingly relevant because of a lack of access to general practice care and the acknowledgement that this activity is and has always been within the scope of practice of a pharmacist in terms of education and training.
‘Pharmacists need to ensure they are competent in terms of their training (vaccination certified, medicines administration training has been completed) and that they inform themselves of the relevant information related to each drug being administered.
 ‘In my view, it’s analogous to dispensing a new drug that you haven’t come across before. You understand the relevant information related to the drug from a safety and effectiveness point of view, you communicate with the patient regarding relevant counselling points, and you document relevant information.’
‘In my view, it’s analogous to dispensing a new drug that you haven’t come across before. You understand the relevant information related to the drug from a safety and effectiveness point of view, you communicate with the patient regarding relevant counselling points, and you document relevant information.’
But the future isn’t just about the administration of a medicine. Rather, Dr Jackson says, this is just the start of pharmacists ‘being more involved and taking more responsibility and accountability for patient care’.
‘Regulatory misunderstanding and regulatory impediments have for a long time prevented pharmacists from doing more in the prescribing, administration and review of medicines.
‘We are seeing these barriers being reduced, albeit slowly in some jurisdictions, to allow pharmacists to do more, to practise to their full scope in terms of medicines management.
‘Ideally, pharmacists should be empowering patients to better take control of their own health care. For most of the medicines we see currently, patients with appropriate support can self-administer,’ says Dr Jackson.
‘In some cases, there may be barriers in place and pharmacists may deliver regular injections for these patients. It’s a case-by-case basis with the patient at the centre of care.’
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28084
[post_author] => 3410
[post_date] => 2024-11-06 15:56:15
[post_date_gmt] => 2024-11-06 04:56:15
[post_content] => After months of anticipation, the Unleashing the potential of our health workforce – Scope of practice review was released yesterday (5 November) – with many of the key recommendations echoing the long-held concerns of the PSA and pharmacists across Australia.
Australian Pharmacist has rounded up some of the key takeouts from the report.
Pharmacists are leaving the profession at an alarming rate
Pharmacy has a high attrition rate compared with other healthcare professions. Among 19 healthcare professions, pharmacy had the fifth highest exit rate of 8.7% in 2023 – almost double that of medical professionals (4.7%).
The professions with the highest exit rates are those that face significant barriers to working to their full scope of practice, the review found.
While there are several factors that impact exit rates, allowing pharmacists to work to their full scope of practice is a crucial factor for strengthening the profession’s retention rate – improving recognition for professional skills, capability and contribution to enhance continuity of care.
‘This report really makes clear that there are all sorts of artificial, inefficient restrictions on what nurses, pharmacists, GPs, and other health professionals are allowed to do that bears no relationship to their training,’ said federal Minister for Health and Aged Care Mark Butler.
Inconsistencies in vaccine schedules for pharmacists are ‘needless’
Pharmacist vaccinators are trained in accordance with the National Immunisation Education Framework, ensuring high standards in vaccine administration and competence.
But the report found that the difference in state and territory laws dictating which vaccines can be administered by pharmacists has led to disparities in access – not only causing confusion among patients but leading to significant inefficiencies.
Legislative differences between states and territories also means that a vaccine subsidised in one region might not be covered in another.
Harmonising these regulations by reviewing Drugs and Poisons Acts would promote equitable vaccine access nationwide, allowing pharmacists’ to provide consistent healthcare services regardless of location.
Aligning funding arrangements for vaccination is also crucial, the review found. While the National Immunisation Program Vaccinations in Pharmacy (NIPVIP) provides government funding for certain vaccines, access to others depends on a mix of user-pay systems and varying jurisdictional funding – creating inconsistencies in affordability and accessibility across states and territories.
Standardising funding mechanisms would ensure subsidies are uniformly applied – making vaccinations more affordable and accessible to all Australians.
It will take some time to implement change, but there are some steps governments and regulators can take now
While some of the recommendations in the review, such as harmonising vaccination legislation, can be achieved in a timely fashion, others are sweeping reforms that will take many years, such as restructuring healthcare education – which currently impacts students and qualified pharmacists’ ability to work to their full scope.
The review recommended the Commonwealth establish a primary care workforce development program to support the development and retention of a skilled, stable, and collaborative primary care workforce through enhanced curriculum, training, placement, and career development opportunities for students, supervisors, mentors, and health professionals.
The current funding model must be overhauled
The current fee-for-service arrangement in primary care incentivises high-turnover care – with payments to providers based on the number and type of care episodes delivered.
This model limits the ability of health professionals to work to their full scope and reduces multidisciplinary collaboration – with some healthcare professionals funded for certain services while others are not, including lack of funding for pharmacists to participate in multidisciplinary case conferences.
To address this, the review recommends introducing a blended payment model to complement the fee-for-service system. This model would enable access to multidisciplinary healthcare delivered by professionals working to their full scope of practice in primary care.
An independent mechanism would be established to advise on pricing and payment levels for the blended payment, ensuring adjustments based on the risk profile of patient populations.
But it’s unlikely to be a quick fix. The review suggests the model would need to be implemented progressively over a 7-year period, beginning with priority areas such as rural and remote regions, Aboriginal Community Controlled Health Organisations, and underserviced regional and outer metropolitan areas.
Pharmacist prescribing programs should be nationally consistent
Implementing pharmacists prescribing rights has been an unnecessarily complex and prolonged process, with ad-hoc investigations, one-off reviews, and small-scale pilots.
Adopting an activity-based approach would streamline regulation for community pharmacists in prescribing medications and promote consistency across jurisdictions.
Introducing a dedicated mechanism to assess health workforce models would also fill a crucial gap, facilitating the systematic adoption of multidisciplinary primary care models that include pharmacists much like the successful models implemented in the United Kingdom.
Improved use of technology should form the backbone of scope of practice changes
A key theme in the review was the need for better use of technology across the board to expand scopes of practice and efficiencies, improving quality of care.
Potential areas for reform identified by the review include establishing access to real‑time patient information, introducing platforms for secure messaging and digital referrals and mandating participation in a multidisciplinary care team for primary care providers.
‘[We need to] improve the digital capability of a system that still uses far too many fax machines and too much paper,’ said Minister Butler.
The government will respond, in time
The government is yet to respond to the key recommendations in the report, with Minister Butler confirming he will not ‘respond to each of the ideas’.
‘We want to consider them, but a lot of them do have a lot of common sense,’ he said.
Other key stakeholders will also need to be consulted.
‘Many of the recommendations will require collaboration between the Commonwealth and state and territory governments, as well as consultation with peak professional organisations, AHPRA, patient groups, and the sector more broadly. I look forward to these discussions,’ Minister Butler added.
But PSA has called for the government to accept all 18 recommendations and put forward a plan of action now.
This review confirms PSA’s view that inconsistent regulations, unnecessary restrictions on practice, and siloed workforces are having a negative impact on patient access to quality health care, said PSA National President Associate Professor Fei Sim.
‘This report recognises the core role of pharmacies and pharmacists as primary healthcare providers and recommends a multidisciplinary approach to patient care,’ she said.
‘There is a clear alignment between Cormack’s recommendations and the actions in PSA’s vision for the pharmacy profession, Pharmacists in 2030. Both present a clear vision for the future that requires collaboration for a health system that works for patients.’
What the health sector is saying
The Australian Medical Association has said that the government ‘must resist’ changes to scope of practice, maintaining its position for even more investment into general practice.
Meanwhile, the Royal Australian College of GPs said the recommendations, if implemented, would ‘raid Medicare’, setting up for a ‘two-tiered health system where those who can afford to see a GP will, and those who can’t, don’t.’
But the Australian Nursing and Midwifery Federation said the review allows highly-trained health professionals to best utilise their skills, education and experience, allowing for the delivery of integrated, quality healthcare services across the community.
Support also came from the National Rural Health Alliance, who welcomed the recommendations that seek to address some of the ‘inequalities faced by rural Australians when it comes to accessing healthcare.’
Outside of the health sector, the Business Council of Australia also welcomed the report, citing improving ‘productivity, patient experience and workforce satisfaction’ as necessary to a sustainable health system.
[post_title] => Key recommendations to strengthen pharmacists’ role in healthcare
[post_excerpt] => The scope of practice review recommends sweeping legislative change and solutions to funding challenges to improve healthcare services.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => key-recommendation-to-strengthen-pharmacists-role-in-healthcare
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-06 17:01:11
[post_modified_gmt] => 2024-11-06 06:01:11
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28084
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Key recommendations to strengthen pharmacists’ role in healthcare
[title] => Key recommendations to strengthen pharmacists’ role in healthcare
[href] => https://www.australianpharmacist.com.au/key-recommendation-to-strengthen-pharmacists-role-in-healthcare/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28086
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28164
[post_author] => 3410
[post_date] => 2024-11-13 12:50:58
[post_date_gmt] => 2024-11-13 01:50:58
[post_content] => The Therapeutic Goods Administration (TGA) has worked with Phenergan manufacturer Sanofi to develop a new contraindication for the medicine in children under 6.
The decision to restrict use of the medicine in this age cohort – commonly used to treat allergies, travel sickness and nausea – is based on a thorough evaluation of new scientific evidence that the risks outweigh the benefits, a spokesperson for Sanofi told Australian Pharmacist.
‘Following recent evaluations made by Sanofi Consumer Healthcare Pty Ltd, including a benefit-risk assessment, the research has shown a causal association between promethazine and safety concerns,’ said this spokesperson.
The sponsor-initiated update was prompted by advice from the TGA Advisory Committee on Medicines (ACM) – first-generation oral sedating antihistamines – do not use in children, said a spokesperson from the TGA.
‘Further review by the sponsor of cumulative safety data in children 2 to 5 years of age demonstrated sufficient evidence of a causal association between promethazine and psychiatric and central nervous system adverse events in this age group,’ the TGA spokesperson told AP.
The contraindication comes after Medsafe, the New Zealand Medicines and Medical Devices Safety Authority, moved to contraindicate the use of the medicine in children under 6 due to the potential for fatal respiratory depression, psychiatric and central nervous system (CNS) events.
AP understands that the contraindication will affect other products. A spokesperson for AFT said a variation has been submitted to update the product information and label on Allersoothe Elixir with a change to the age indication from children 2 years and older to children 6 years and older. This submission is pending approval.
Will the packaging change?
Not immediately.
New labels for promethazine-containing products will be rolled out in 2025 due to production and logistics lead times, said the Sanofi spokesperson.
‘No immediate action is required regarding current stock. There is no need to set aside existing medications, as this communication does not constitute a recall,’ said the spokesperson. ‘Similarly, the revised labels do not create any changes in the ordering process.
The product information for Phenergan has been updated and is available here.
What should pharmacists do if they get a Phenergan script for an 18 month old infant?
The use of promethazine in children under 6 years of age is now both contraindicated and off label, said Peter Guthrey MPS, PSA Senior Pharmacist – strategic policy.
‘This means that if you choose to dispense, both the prescriber and dispenser carry the full indemnity risk, and you need to get the patient to provide informed consent,’ he said.
Should a parent present with a script for promethazine for use in a child under 6 years of age, pharmacists should contact the prescriber to discuss the risks and benefits, noting that it's contraindicated.
Is there any situation where it would be appropriate to dispense Phenergan to a young child?
It would need to be a pretty compelling case, where the benefit to a child outweighed the risk of respiratory depression, psychiatric or CNS events , said Mr Guthrey.
‘Given it’s a documented contraindication, it'd be pretty hard to demonstrate the medicine is ‘‘safe and therapeutically appropriate’’,’ he said.
‘It is going to be difficult to find a situation where supply is clinically justified and pharmacists have met their obligations to patient safety.’
What about prescribing Phenergan as a Schedule 3 medicine?
If a parent requests promethazine as a Schedule 3 medicine for someone under the age of 6 years, generally alternate products or advice for treatment should be provided following a discussion.
‘While a pharmacist prescribing promethazine as a Pharmacist Only Medicine is lawful for children aged 2-5 years, it is still contraindicated,’ said Mr Guthrey. ‘There would be very few, if any, situations where prescribing the medicine where contraindicated would be warranted.’
What about phenylephrine?
There are some combination phenylephrine products indicated for children under 6 years of age for nasal congestion. However, there is plenty of evidence showing that oral phenylephrine products are ineffective as a nasal decongestant.
In fact, the United States Food and Drug Administration (FDA) recently announced it will move to ban oral phenylephrine products because they simply don't work.
‘Based on our review of available data, and consistent with the advice of the advisory committee, we are taking this next step in the process to propose removing oral phenylephrine because it is not effective as a nasal decongestant,’ said Patrizia Cavazzoni, M.D., director of the FDA’s Center for Drug Evaluation and Research .
While a spokesperson for the TGA told Australian Pharmacist back in July that there are ‘no plans’ to review the effectiveness of oral phenylephrine, it will continue to monitor the outcomes of the FDA review.
What advice should pharmacists provide?
For children with allergies, non-sedating histamines are first line.
The best thing parents can do when a child under 6 years of age has cough or cold symptoms is to wait it out, with a review by a medical practitioner when appropriate.
‘It's about reassurance to parents that the cough in itself isn't harmful, and that kids don’t always need medicines for a cold – they need time and supportive therapy,’ said Mr Guthrey.
It’s important that pharmacists give parents confidence that they're doing the right thing by not treating the cough, and providing symptomatic relief for fever and chills, and ensuring they are appropriately counselled on when review by a medical practitioner may be appropriate.
For more information, refer to the Australian Pharmaceutical Formulary and Handbook treatment guidelines on:
[post_title] => Do not supply Phenergan to children under 6, manufacturer warns
[post_excerpt] => The TGA has worked with Phenergan manufacturer Sanofi to develop a new contraindication for the medicine in children under 6.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => do-not-supply-phenergan-to-children-under-6-manufacturer-warns
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-13 16:15:31
[post_modified_gmt] => 2024-11-13 05:15:31
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28164
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Do not supply Phenergan to children under 6, manufacturer warns
[title] => Do not supply Phenergan to children under 6, manufacturer warns
[href] => https://www.australianpharmacist.com.au/do-not-supply-phenergan-to-children-under-6-manufacturer-warns/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28167
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28142
[post_author] => 3410
[post_date] => 2024-11-11 15:55:46
[post_date_gmt] => 2024-11-11 04:55:46
[post_content] => With cases of Respiratory syncytial virus (RSV) spiking this year, the federal government announced yesterday (10 November) that free vaccination would be offered to eligible pregnant people and babies.
Before the 2025 winter season, the RSV vaccine will be available under the National Immunisation Program (NIP) for all people in the third trimester of pregnancy via the Australian Infant RSV Immunisation Program.
Which RSV vaccines will pharmacists administer?
The RSV immunisation program will offer two Therapeutic Goods Administration approved protections against severe RSV.
Pharmacists can administer the maternal vaccine, Abrysvo, to pregnant women between 28-36 weeks of gestation.
Maternal vaccination provides early protection for newborn children by reducing the risk of severe RSV disease in infants under 6 months of age by around 70%, a spokesperson from the Department of Health and Aged Care told Australian Pharmacist.
‘This is [through] passive protection by transplacental transfer of RSV-specific antibodies from the mother to the foetus during pregnancy.’
How popular will it be?
Federal Minister for Health and Aged Care Mark Butler said the RSV vaccine rollout has been modelled on the whooping cough vaccine in pregnant women, which is administered at around the same time and has an uptake rate of around 80%.
‘Maternal vaccination provides early protection for newborn children by reducing the risk of severe RSV disease in infants under 6 months of age by around 70%.'
The Department of Health and Aged Care
‘So we have good confidence that there will be a significant uptake of this maternal vaccine by pregnant Australian women,’ he added.
What is covered for pharmacists under the NIP?
According to the Department of Health and Aged Care, both the cost of the maternal RSV vaccine (Abrysvo) and the vaccine administration fee will be covered under the NIP and The National Immunisation Program Vaccinations in Pharmacy (NIPVIP) Program.
Abrysvo NIP vaccine stock will also be available to community pharmacists, said the spokesperson.
What about protection for neonates?
Access has also widened for more babies to receive a protection against RSV soon after birth, particularly those whose mother did not opt to have the vaccine during pregnancy.
Beyfortus (nirsevimab), an antibody therapy for the prevention of RSV-related lower respiratory tract disease, will be available in hospitals, immunisation clinics and general practices for infants before or during their first RSV season. Children up to 24 months of age who remain vulnerable to severe RSV disease throughout their second RSV season can also access the vaccine.
‘Beyfortus is a monoclonal antibody treatment which is administered to babies by injection,’ said Minister Butler. ‘[It can be received] immediately after birth … if their mother has not been vaccinated against RSV.’
Why did the government decide to take action against RSV?
Australia recorded the highest ever number of RSV cases this year, with 165,910 reported notifications.
Most cases were recorded in the 0–4 age cohort, among whom RSV can be fatal, and is the leading cause of hospitalisation for Australian children under five years of age.
The Australian Immunisation Foundation estimates that around 12,000 Australian babies aged 12 months or younger are admitted to hospital with RSV annually. Around 25% of these children will require intensive care.
The inclusion of an RSV vaccine in the NIP is an important step to protect newborn children and infants from severe RSV infection, said the spokesperson.
‘The highest rate of RSV-related hospitalisations is in infants during their first few months of life,’ said the spokesperson.
‘Infants with medical risk factors, such as being born very [premature], under 32 weeks gestational age, have an increased risk of severe disease.
‘Up to 80% of infants who are hospitalised due to RSV are otherwise healthy children with no predisposing conditions.’
What’s the expected impact?
The Immunisation Foundation of Australia has estimated that the nationwide availability of new RSV immunisations will help to keep 10,000 infants out of hospital with related bronchiolitis or pneumonia each year.
‘The immunisations being funded in Australia protect babies against severe RSV and have been shown to slash hospitalisation rates by up to 90 per cent,’ said Catherine Hughes AM, Founder and Director of the Immunisation Foundation of Australia.
Western Australia was the first state to implement an infant RSV immunisation program with Beyfortus. More than 23,000 infants received RSV protection this year, resulting in up to 84% fewer hospitalisations in immunised newborns compared to those who were not RSV protected. In Queensland, where a statewide infant RSV immunisation program commenced in April 2024, similar results were observed.
‘The exceptional results in Western Australia and Queensland contrast sharply with other parts of Australia where hospitals were overwhelmed by babies struggling to breathe due to severe RSV,’ she said.
Will older patients be able to receive the RSV vaccine under the NIP?
No. Well at least, not yet.
Vaccines can only be listed on the NIP after a positive recommendation from the Pharmaceutical Benefits Advisory Committee’s (PBAC) as required by the National Health Act 1953, said the spokesperson.
‘Several vaccine sponsors have made submissions in relation to RSV vaccines for older populations to the PBAC to consider for NIP listing,’ said the spokesperson.
‘The outcomes of these meetings will inform future government considerations regarding the potential listing of RSV vaccines on the NIP for older Australians.’
While a positive PBAC recommendation is an essential requirement in the NIP-listing process, other steps need to be completed before a vaccine can be given final approval for NIP listing, said the spokesperson.
‘These include negotiations with the relevant pharmaceutical company, finalisation of conditions for listing, quality and availability checks and final consideration by the government,’ said the spokesperson. ‘These considerations and decisions of government cannot be preempted.’
[post_title] => Government-funded RSV vaccines to protect infants from severe disease
[post_excerpt] => With cases of RSV spiking in 2024, the federal government announced free vaccination would be offered to eligible pregnant people and babies.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => government-funded-rsv-vaccines-to-protect-infants-from-severe-disease
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-13 13:26:32
[post_modified_gmt] => 2024-11-13 02:26:32
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28142
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Government-funded RSV vaccines to protect infants from severe disease
[title] => Government-funded RSV vaccines to protect infants from severe disease
[href] => https://www.australianpharmacist.com.au/government-funded-rsv-vaccines-to-protect-infants-from-severe-disease/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28146
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28134
[post_author] => 9164
[post_date] => 2024-11-11 12:48:48
[post_date_gmt] => 2024-11-11 01:48:48
[post_content] => Pharmacists and migrant community leaders, Sobia Hashmi MPS and Irfan Hashmi MPS, are the 2025 Local Heroes for South Australia, receiving their award on Saturday night in a ceremony in Adelaide.
The local heroes category of these Australia Day awards recognise role models who encourage others to be active in their own communities and become agents of positive change for a more diverse and inclusive Australia.
Over 20 years, Sobia and husband Irfan have transformed healthcare in remote and rural communities in South Australia. They’ve established six pharmacies in areas where there were previously none – which forced people to travel long distances for life-saving medicines and primary health care.
Sobia (48) and Irfan (51) are committed to serving their diverse communities. They employ staff who collectively speak 21 languages, allowing them to reach vulnerable populations and provide culturally sensitive healthcare. In 2020, they partnered with government to provide 24 free influenza vaccine clinics in outreach settings, providing 1200 vaccines to vulnerable people in South Australia.
Reflecting on the awards, Irfan and Sobia told Australian Pharmacist that the award was a celebration of the collective efforts of everyone who has been with them along the way, including their family, friends, colleagues, and the broader community.
‘To every individual who believed in us, who encouraged us to reach higher, and who shared in our vision of uplifting others, thank you. Your unwavering support drives us to do more, reach further, and connect deeper with those around us,’ they said.
Sobia and Irfan also reflected on the importance of community.
‘Together, we are stronger. Together, we make a difference. And together, let’s continue to build a healthier, more inclusive South Australia for all. This is just the beginning, and we are excited for the journey ahead,’ they said.
‘We are truly honoured and humbled to be named the 2025 Australian of the Year Award – Local Hero in SA recipients. This recognition strengthens our commitment to making a positive impact as pharmacists and community leaders, and it inspires us to continue serving the vibrant multicultural community that we call home.’
The couple have mentored countless intern pharmacists from overseas, coordinating multilingual education and outreach initiatives to help pharmacists enter the much-needed workforce in regional Australia. They host a free weekly webinar series, which has assisted 4,000 overseas pharmacists in passing their registration exams in the last 12 months alone.
Irfan previously was recognised as PSA’s 2009 South Australian Pharmacist of the Year.
[post_title] => Two pharmacists win state Australian of the Year 2025 award
[post_excerpt] => Sobia Hashmi MPS and Irfan Hashmi MPS will attend the Australian of the Year awards as finalists for the national local heroes title.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => two-pharmacists-win-state-australian-of-the-year-2025-award
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-13 13:26:46
[post_modified_gmt] => 2024-11-13 02:26:46
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28134
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Two pharmacists win state Australian of the Year 2025 award
[title] => Two pharmacists win state Australian of the Year 2025 award
[href] => https://www.australianpharmacist.com.au/two-pharmacists-win-state-australian-of-the-year-2025-award/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28140
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 27932
[post_author] => 235
[post_date] => 2024-11-07 00:53:00
[post_date_gmt] => 2024-11-06 13:53:00
[post_content] => A megatrend has begun in medicines. The increasingly large and full fridges found in pharmacies stand as a testament to the growing prevalence of injectable medicines – and are a sign of things to come.
In the near future, many daily tablets may be replaced with periodic appointments to have a medicine administered by injection.
The injectables are coming
Options for injectables and other non-oral dose forms such as patches, gels and sprays are rapidly growing, with these increasingly replacing medicinal therapies delivered through swallowing tablets, capsules or liquids. Pharmacists will recognise these examples.
Prolia (denosumab), which has been registered for the treatment of osteoporosis in Australia since 2010, offers a glimpse of the future, replacing daily or weekly tablets with biannual injections.1 Similarly, the relatively new cholesterol-lowering drug Leqvio (inclisiran) is administered every 6 months as a maintenance dose, after the initial induction doses, offering a new route for lipid modifying therapy.2
And Eli Lilly has a new US Food and Drug Administration-approved injectable, Kisunla (donanemab-azbt), coming out for the treatment of Alzheimer’s disease (AD).3 Delivered by infusion every 4 weeks, the drug works by targeting deposits of amyloid plaque in the brain, which is a key indicator of the presence of the debilitating, ultimately fatal brain disease.
Last month, one of the world leaders in AD research, Professor Colin Masters of The Florey Institute of Neuroscience and Mental Health in Melbourne, told neurologists and healthcare workers who treat patients with progressive neurodegenerative diseases of promising results from the Roche Dominant Inherited Alzheimer’s Network (DIAN) trial of the monoclonal antibody gantenerumab. Roche’s “Brain Shuttle” technology is now being used to cross the blood-brain barrier and then clear amyloid plaque aggregation with a newer generation, bio-specific, monoclonal antibody called trontinemab.
Prof Masters told a Creutzfeldt-Jakob Disease Support Group Network (CJDSGN)workshop on CJD and other prion diseases that early results from a trial of trontinemab are currently in pre-press in The Lancet.⁴

It’s also hoped, he says, that current intravenous AD drug models may evolve to be delivered subcutaneously via an autoinjector by patients at home.
Perhaps most revolutionary, however, are the advancements in HIV prevention. Recently, research into Gilead’s long-acting injection, lenacapavir (an agent for treatment of HIV), has shown promising results in pre-exposure prophylaxis (PrEP), and has been described as ‘the closest we have ever been to an HIV vaccine’ .⁵ At the AIDS 2024 conference in Germany in July, researchers presented their findings that twice-yearly lenacapavir demonstrated 100% efficacy for HIV prevention in cisgender women.⁶
‘The pace at which innovative, new medicines are entering the market is unprecedented,’ says Medicines Australia CEO Liz de Somer. ‘Advances in research, technology and innovation mean we can expect to see new forms of treatments – which include innovative new medicines and improved forms of existing medicines – becoming available.’
These are huge leaps forward in how health is treated, and pharmacists will need to adapt, says PSA National Board member Dr Shane Jackson FPS, community and credentialed pharmacist and lecturer in pharmacy at the University of Tasmania.
‘Medicines have always been an evolving space. Research on mRNA-delivered therapeutics has actually been around for about 20 years, and the pipeline of mRNA therapeutics is and will be a gamechanger in terms of treatment and prevention of disease in the future,’ he says.
‘What this means is that pharmacists will be needed more than ever because of their deep expertise in the use of medicines, and the term “medicines experts” will most likely evolve to “therapeutics experts”, noting the change from “medicine” to the complete management and prevention of disease.’
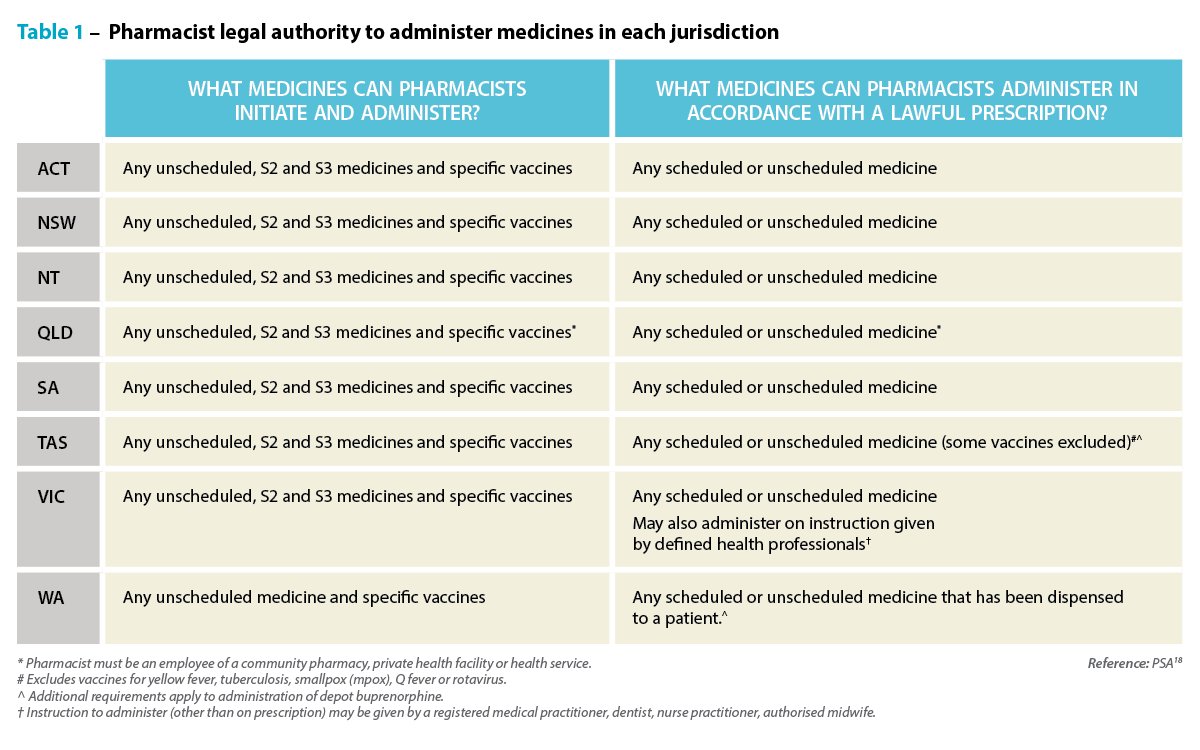 New formats needed
New formats needed
One reason alternative delivery systems like injections and patches are becoming more prevalent is because they are critical for delivering new, biologically complex drugs.
As scientists have developed new treatments, they have created molecules that are too large or sensitive to be absorbed effectively through the digestive system. For example, Humira (adalimumab), the monoclonal antibody used to treat autoimmune conditions including juvenile arthritis and Crohn’s disease, is administered through subcutaneous injection because its large molecular structure would be ineffective if taken orally.⁷
Or take the testosterone transdermal delivery patch Androderm.8 Delivering testosterone directly through the skin provides a steady hormone level that can’t be achieved with oral testosterone.⁹
Technological advancements in mRNA technology, showcased in the production of COVID-19 vaccines, are also driving treatments and other preventive measures for different conditions.
‘Prior to the pandemic, mRNA-based drug products were focused primarily on treating oncology indications as opposed to infectious diseases, such as COVID-19,’ says Martin Gonzalez, Pfizer’s senior manager of product development.10
‘However, technical and scientific advancements have allowed researchers and drug developers to expand the use of mRNA to new therapeutic areas.’
For patients who inject themselves daily, there is also a growing preference for better ways to self-administer medicines. This focus on the patient has led to advances in medical devices in recent decades, introducing prefilled syringes, pens and automated electronic and infusion devices.

‘Much of the emphasis in contemporary drug design has shifted from just preserving basic quality attributes, such as safety, efficacy and potency, in a simple container,’ Mr Gonzalez says.10
‘Today’s [sterile injectable] drugs carry a more complex profile and incorporate new thinking about ways of preserving the value of the drug while also providing additional benefits, including precise, easy-to-administer delivery systems for better dose compliance.’
Improving medicine adherence
According to the World Health Organization, around 50% of patients with chronic illnesses in developed countries don’t take their medicines as prescribed.11
The rates are even lower in developing nations. There are myriad reasons for poor medicine adherence, including low health literacy, the prescription of complex drug regimens and limited access to care.12
Long-acting therapies may also be beneficial for hard-to-reach populations, such as those experiencing homelessness or substance use problems. And in the case of those living with HIV, long-acting drugs might also be useful for children, says Dr Charles Flexner, HIV expert at Johns Hopkins University. Globally, just 50% of children diagnosed with HIV are receiving treatment, in part due to a lack of drug versions made for children.13
‘With long-acting formulations, that will no longer be the case,’ Dr Flexner says.13 ‘Children will be able to use the same formulation as adults, just at a different dose.’
Breakthrough in injectable PrEPLong-acting injectables for HIV treatment and prevention are providing convenience, promoting better adherence, and helping to reduce the stigma and discrimination that might come with taking a daily pill.14 In Australia, there is currently one injectable HIV medicine listed on the Pharmaceutical Benefits Scheme (PBS) – Cabenuva (cabotegravir/rilpivirine), which requires injections every 2 months.15 Cabotegravir-LA for pre-exposure prophylaxis (PrEP) has been approved by the Therapeutic Goods Administration (TGA) but is not yet listed on the PBS,16 and lenacapavir is also TGA-approved but not PBS listed for treating multidrug-resistant HIV in combination with other antiretroviral therapy. Globally, 6-monthly injections of lenacapavir have also been trialled for PrEP, with extraordinary results. Clinical trial data released this year in a study of cisgender men, transgender men, transgender women, and nonbinary individuals who have sex with partners assigned male at birth showed that using lenacapavir results in a 96% lower HIV rate compared with the expected incidence of infection, and an 89% lower HIV rate compared with oral PrEP.17
Trials have also shown an efficacy rate of 100% among cisgender women in South Africa and Uganda.
Professor Sharon Lewin, Director of the Peter Doherty Institute for Infection and Immunity at the University of Melbourne, and immediate past president of the International AIDS Society, described the results as ‘a breakthrough advance with huge public health potential’.
‘If approved and delivered – rapidly, affordably and equitably – to those who need or want it, this long-acting tool could help accelerate global progress in HIV prevention,’ Professor Lewin said.⁶
When it comes to long-acting injectables for HIV treatment and prevention: watch this space. Clinical trial data released this year in a study of cisgender men, transgender men, transgender women, and nonbinary individuals who have sex with partners assigned male at birth showed that using lenacapavir results in a 96% lower HIV rate compared with the expected incidence of infection, and an 89% lower HIV rate compared with oral PrEP.17
Trials have also shown an efficacy rate of 100% among cisgender women in South Africa and Uganda.
Professor Sharon Lewin, Director of the Peter Doherty Institute for Infection and Immunity at the University of Melbourne, and immediate past president of the International AIDS Society, described the results as ‘a breakthrough advance with huge public health potential’.
‘If approved and delivered – rapidly, affordably and equitably – to those who need or want it, this long-acting tool could help accelerate global progress in HIV prevention,’ Professor Lewin said.⁶
When it comes to long-acting injectables for HIV treatment and prevention: watch this space. |
As more injectable medicines come onto the market, the pharmacy of the near future will need more consultation rooms and more dispensary refrigerator space.
Pharmacy practice will likely involve more direct patient care, including administering injections and managing complex treatment regimens. Those who fail to adapt, for example by not learning to inject safely, risk becoming obsolete, as the profession increasingly shifts to a more hands-on role.
‘In terms of medicines administration [by injection], this is a newish activity that pharmacists are undertaking,’ Dr Jackson points out. ‘It is becoming increasingly relevant because of a lack of access to general practice care and the acknowledgement that this activity is and has always been within the scope of practice of a pharmacist in terms of education and training.
‘Pharmacists need to ensure they are competent in terms of their training (vaccination certified, medicines administration training has been completed) and that they inform themselves of the relevant information related to each drug being administered.
 ‘In my view, it’s analogous to dispensing a new drug that you haven’t come across before. You understand the relevant information related to the drug from a safety and effectiveness point of view, you communicate with the patient regarding relevant counselling points, and you document relevant information.’
‘In my view, it’s analogous to dispensing a new drug that you haven’t come across before. You understand the relevant information related to the drug from a safety and effectiveness point of view, you communicate with the patient regarding relevant counselling points, and you document relevant information.’
But the future isn’t just about the administration of a medicine. Rather, Dr Jackson says, this is just the start of pharmacists ‘being more involved and taking more responsibility and accountability for patient care’.
‘Regulatory misunderstanding and regulatory impediments have for a long time prevented pharmacists from doing more in the prescribing, administration and review of medicines.
‘We are seeing these barriers being reduced, albeit slowly in some jurisdictions, to allow pharmacists to do more, to practise to their full scope in terms of medicines management.
‘Ideally, pharmacists should be empowering patients to better take control of their own health care. For most of the medicines we see currently, patients with appropriate support can self-administer,’ says Dr Jackson.
‘In some cases, there may be barriers in place and pharmacists may deliver regular injections for these patients. It’s a case-by-case basis with the patient at the centre of care.’
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28084
[post_author] => 3410
[post_date] => 2024-11-06 15:56:15
[post_date_gmt] => 2024-11-06 04:56:15
[post_content] => After months of anticipation, the Unleashing the potential of our health workforce – Scope of practice review was released yesterday (5 November) – with many of the key recommendations echoing the long-held concerns of the PSA and pharmacists across Australia.
Australian Pharmacist has rounded up some of the key takeouts from the report.
Pharmacists are leaving the profession at an alarming rate
Pharmacy has a high attrition rate compared with other healthcare professions. Among 19 healthcare professions, pharmacy had the fifth highest exit rate of 8.7% in 2023 – almost double that of medical professionals (4.7%).
The professions with the highest exit rates are those that face significant barriers to working to their full scope of practice, the review found.
While there are several factors that impact exit rates, allowing pharmacists to work to their full scope of practice is a crucial factor for strengthening the profession’s retention rate – improving recognition for professional skills, capability and contribution to enhance continuity of care.
‘This report really makes clear that there are all sorts of artificial, inefficient restrictions on what nurses, pharmacists, GPs, and other health professionals are allowed to do that bears no relationship to their training,’ said federal Minister for Health and Aged Care Mark Butler.
Inconsistencies in vaccine schedules for pharmacists are ‘needless’
Pharmacist vaccinators are trained in accordance with the National Immunisation Education Framework, ensuring high standards in vaccine administration and competence.
But the report found that the difference in state and territory laws dictating which vaccines can be administered by pharmacists has led to disparities in access – not only causing confusion among patients but leading to significant inefficiencies.
Legislative differences between states and territories also means that a vaccine subsidised in one region might not be covered in another.
Harmonising these regulations by reviewing Drugs and Poisons Acts would promote equitable vaccine access nationwide, allowing pharmacists’ to provide consistent healthcare services regardless of location.
Aligning funding arrangements for vaccination is also crucial, the review found. While the National Immunisation Program Vaccinations in Pharmacy (NIPVIP) provides government funding for certain vaccines, access to others depends on a mix of user-pay systems and varying jurisdictional funding – creating inconsistencies in affordability and accessibility across states and territories.
Standardising funding mechanisms would ensure subsidies are uniformly applied – making vaccinations more affordable and accessible to all Australians.
It will take some time to implement change, but there are some steps governments and regulators can take now
While some of the recommendations in the review, such as harmonising vaccination legislation, can be achieved in a timely fashion, others are sweeping reforms that will take many years, such as restructuring healthcare education – which currently impacts students and qualified pharmacists’ ability to work to their full scope.
The review recommended the Commonwealth establish a primary care workforce development program to support the development and retention of a skilled, stable, and collaborative primary care workforce through enhanced curriculum, training, placement, and career development opportunities for students, supervisors, mentors, and health professionals.
The current funding model must be overhauled
The current fee-for-service arrangement in primary care incentivises high-turnover care – with payments to providers based on the number and type of care episodes delivered.
This model limits the ability of health professionals to work to their full scope and reduces multidisciplinary collaboration – with some healthcare professionals funded for certain services while others are not, including lack of funding for pharmacists to participate in multidisciplinary case conferences.
To address this, the review recommends introducing a blended payment model to complement the fee-for-service system. This model would enable access to multidisciplinary healthcare delivered by professionals working to their full scope of practice in primary care.
An independent mechanism would be established to advise on pricing and payment levels for the blended payment, ensuring adjustments based on the risk profile of patient populations.
But it’s unlikely to be a quick fix. The review suggests the model would need to be implemented progressively over a 7-year period, beginning with priority areas such as rural and remote regions, Aboriginal Community Controlled Health Organisations, and underserviced regional and outer metropolitan areas.
Pharmacist prescribing programs should be nationally consistent
Implementing pharmacists prescribing rights has been an unnecessarily complex and prolonged process, with ad-hoc investigations, one-off reviews, and small-scale pilots.
Adopting an activity-based approach would streamline regulation for community pharmacists in prescribing medications and promote consistency across jurisdictions.
Introducing a dedicated mechanism to assess health workforce models would also fill a crucial gap, facilitating the systematic adoption of multidisciplinary primary care models that include pharmacists much like the successful models implemented in the United Kingdom.
Improved use of technology should form the backbone of scope of practice changes
A key theme in the review was the need for better use of technology across the board to expand scopes of practice and efficiencies, improving quality of care.
Potential areas for reform identified by the review include establishing access to real‑time patient information, introducing platforms for secure messaging and digital referrals and mandating participation in a multidisciplinary care team for primary care providers.
‘[We need to] improve the digital capability of a system that still uses far too many fax machines and too much paper,’ said Minister Butler.
The government will respond, in time
The government is yet to respond to the key recommendations in the report, with Minister Butler confirming he will not ‘respond to each of the ideas’.
‘We want to consider them, but a lot of them do have a lot of common sense,’ he said.
Other key stakeholders will also need to be consulted.
‘Many of the recommendations will require collaboration between the Commonwealth and state and territory governments, as well as consultation with peak professional organisations, AHPRA, patient groups, and the sector more broadly. I look forward to these discussions,’ Minister Butler added.
But PSA has called for the government to accept all 18 recommendations and put forward a plan of action now.
This review confirms PSA’s view that inconsistent regulations, unnecessary restrictions on practice, and siloed workforces are having a negative impact on patient access to quality health care, said PSA National President Associate Professor Fei Sim.
‘This report recognises the core role of pharmacies and pharmacists as primary healthcare providers and recommends a multidisciplinary approach to patient care,’ she said.
‘There is a clear alignment between Cormack’s recommendations and the actions in PSA’s vision for the pharmacy profession, Pharmacists in 2030. Both present a clear vision for the future that requires collaboration for a health system that works for patients.’
What the health sector is saying
The Australian Medical Association has said that the government ‘must resist’ changes to scope of practice, maintaining its position for even more investment into general practice.
Meanwhile, the Royal Australian College of GPs said the recommendations, if implemented, would ‘raid Medicare’, setting up for a ‘two-tiered health system where those who can afford to see a GP will, and those who can’t, don’t.’
But the Australian Nursing and Midwifery Federation said the review allows highly-trained health professionals to best utilise their skills, education and experience, allowing for the delivery of integrated, quality healthcare services across the community.
Support also came from the National Rural Health Alliance, who welcomed the recommendations that seek to address some of the ‘inequalities faced by rural Australians when it comes to accessing healthcare.’
Outside of the health sector, the Business Council of Australia also welcomed the report, citing improving ‘productivity, patient experience and workforce satisfaction’ as necessary to a sustainable health system.
[post_title] => Key recommendations to strengthen pharmacists’ role in healthcare
[post_excerpt] => The scope of practice review recommends sweeping legislative change and solutions to funding challenges to improve healthcare services.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => key-recommendation-to-strengthen-pharmacists-role-in-healthcare
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-06 17:01:11
[post_modified_gmt] => 2024-11-06 06:01:11
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28084
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Key recommendations to strengthen pharmacists’ role in healthcare
[title] => Key recommendations to strengthen pharmacists’ role in healthcare
[href] => https://www.australianpharmacist.com.au/key-recommendation-to-strengthen-pharmacists-role-in-healthcare/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28086
[authorType] =>
)






Get your weekly dose of the news and research you need to help advance your practice.
Protected by Google reCAPTCHA v3.

Australian Pharmacist is the official journal for Pharmaceutical Society of Australia Ltd.










