Christmas came early for pharmacists and patients this year, with the Minister for Health and Aged Care, the Hon Mark Butler yesterday releasing an updated version of the National Medicines Policy (NMP).
Welcoming the changes and congratulating Deputy Chief Medical Officer Professor Michael Kidd AM on the improved policy, PSA National President Dr Fei Sim said the revision meets the contemporary needs of Australians.
‘Medicines are our most common intervention in health care,’ she said. ‘It is essential that Australians have access to quality and affordable medicines when they need them.’
Echoing Dr Sim, Prof Kidd told Australian Pharmacist that the inclusion of a strong vision statement and expansion of the principle of equity recognises that all Australians should have timely, safe and affordable access to high-quality medicines and medicines-related services.

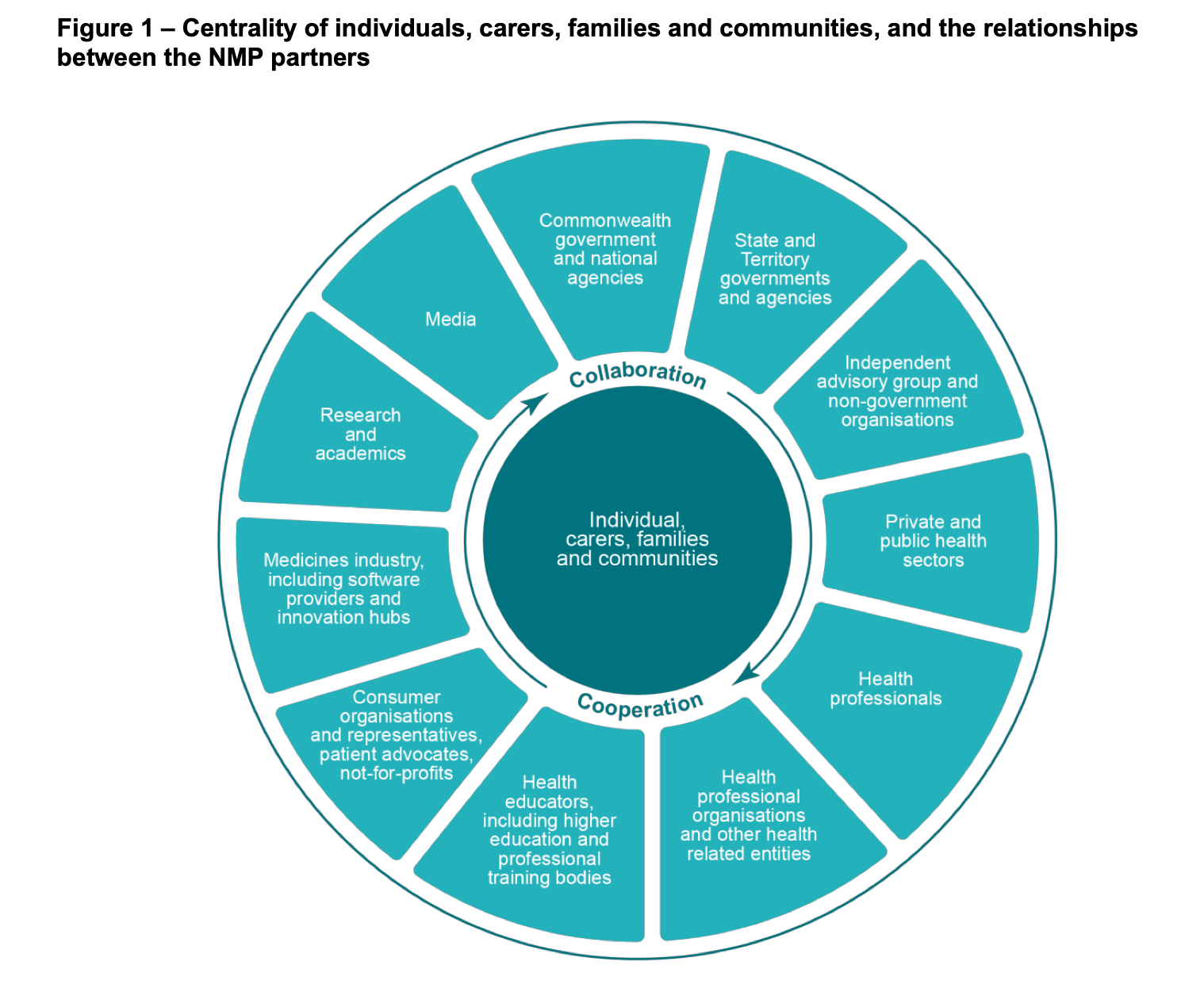
‘This policy guides and focuses the efforts of all partners to encourage greater dialogue, collaboration and cooperation in achieving the vision and aim of the policy for the benefit of all Australians,’ he said.
The updates to the NMP come after years of advocacy from PSA – particularly after ‘Quality Use of Medicines and Medicines Safety’ was declared the 10th National Health Priority Area back in 2019.
‘It’s time to review the NMP and make sure it reflects contemporary healthcare needs and practices,’ said PSA’s president at the time Associate Professor Chris Freeman.
What are the changes?
While the NMP is a framework for ensuring Australians have timely access to medicines that are used appropriately, the revised document has a renewed focus on patient-centred care.
‘The updated policy further emphasises the quality use of medicines, medicines safety, and equity, affordability and timeliness of access,’ said Dr Sarah Dineen-Griffin MPS, who is part of the Expert Advisory Committee alongside Emeritus Professor Lloyd Sansom AO FPS, David Herd, and Jan Donovan.
‘It also highlights the importance of delivering positive ways to eliminate health inequities that are experienced by vulnerable population groups within the community.’
This includes addressing barriers to access faced by patient cohorts including Aboriginal and Torres Strait Islander peoples, children and older people, rural and remote communities, people living with disability and those with mental illness.
Another key update is the support for national pharmacovigilance systems.
While embraced by the PSA, Dr Sim said: ‘It’s crucial these systems are nationally coordinated and real-time in order to significantly reduce harms which can be caused by medicines.
‘We also welcome the recognition that clinical indicators will need to be used to evaluate policy, as this is something else PSA has been fighting for over many years.’
Lastly, the NMP also supports world-class innovation and research into new treatments, medicines and medicine services in Australia.
The refreshed plan aligns closely with PSA’s Pharmacists in 2023 report, where patient care is supported by pharmacists as medicine experts wherever medicines are prescribed, supplied or administered.
The changes further provide an opportunity for pharmacists to engage with the Government to ensure the key outcomes of the policy are achieved, Dr Dineen-Griffin said.
‘For example, the profession needs to actively involve itself in not only determining clinical indicators but be part of the measurement and implementation process.’
Constant evolution is necessary
Because the health system and medicines environment experiences continuous change, the NMP must reflect health needs as well as respond to the pace of scientific and technological innovation, said Dr Dineen-Griffin.

‘Flexibility and adaptability within the policy are important to ensure its sustainability and [that] it remains relevant and responsive to the future health environment,’ she said.
To that end, Minister Butler has committed to regular 5-yearly reviews to ensure the NMP remains up to date.
[However], ensuring sufficient representation of all stakeholders in future reviews will be critical,’ adds Dr Dineen-Griffin.Collaboration is key
‘Partnership and shared responsibility’ along with ‘accountability and transparency’ are two fundamental principles within the updated NMP. Only through partners working together will the aim of the policy be achieved, said Dr Dineen-Griffin.
‘Collaboration must recognise the contribution each partner makes to the health, social and economic outcomes for all Australians,’ she said.
Better alignment between policy, legislation and regulatory frameworks across different levels of government is also essential.
‘To further strengthen the policy, high-level performance indicators should be defined and considered,’ she added.
‘We are excited to see changes in policy that should help drive solutions and improve medicine safety for all Australians, and look forward to partnering with the government and other organisations to deliver on the goals of this policy,’ said Dr Sim.
Read the revised NMP to find out more about how the changes impact pharmacists and patients.






 Grace Quach MPS[/caption]
Grace Quach MPS[/caption]






