The significant rise in Australian asthma deaths is cause for immediate and widespread concern. Here’s what experts say needs to change.
Asthma deaths are again on the rise, revealed new Australian Bureau of Statistics data recently released by the National Asthma Council Australia.
There were 467 asthma-related deaths in Australia in 2022, up from 355 deaths in 2021. Most (64%) were among women – with 299 female deaths versus 168 male deaths.
Those most at risk of death are women aged 75 and older, accounting for 45% of all deaths followed by men in this age group (18%).
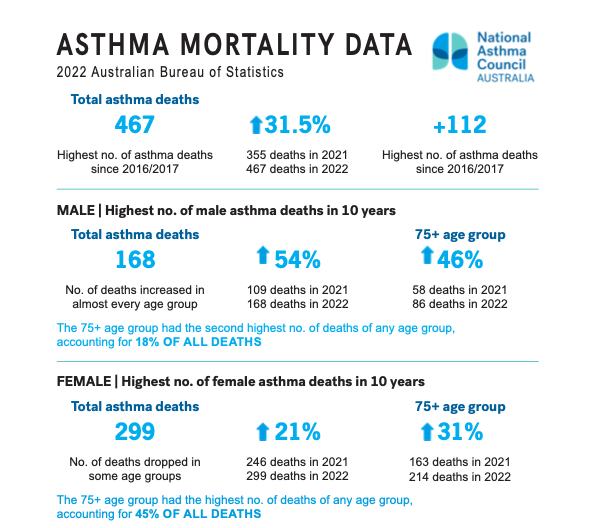 This is the highest number of asthma deaths recorded since 2016-2017. Deaths were down in 2021 as a result of COVID-19 restrictions and lockdowns – leading to fewer respiratory infections and asthma exacerbations. However, asthma exacerbations have now returned to pre-pandemic levels and may even be slightly higher, warned National Asthma Council Australia Director and respiratory physician, Professor Peter Wark.
This is the highest number of asthma deaths recorded since 2016-2017. Deaths were down in 2021 as a result of COVID-19 restrictions and lockdowns – leading to fewer respiratory infections and asthma exacerbations. However, asthma exacerbations have now returned to pre-pandemic levels and may even be slightly higher, warned National Asthma Council Australia Director and respiratory physician, Professor Peter Wark.

This may be the result of the increase in virus infections we saw following the easing of COVID-19 restrictions but the main reasons are a result of the intrinsic problems underlying asthma management in Australia. ‘We’re not accurately diagnosing asthma, and we are under-treating it,’ he said.
A need for better asthma diagnosis and control
There was a marked decline in lung function testing during COVID-19. Despite an increase in funding under the Medicare Benefits Schedule for spirometry, there has been a reduction of two thirds in spirometry being billed under the MBS compared to 2018–19, said Prof Wark.
‘Spirometry remains essential in the diagnosis of asthma and this will lead to under and overdiagnosis,’ said Prof Wark.
Up to 20% of people who present to a pharmacy for salbutamol haven’t had their asthma confirmed by spirometry, said Advanced Practice Pharmacist and National Asthma Council Australia Clinical Executive Lead Debbie Rigby FPS.
‘Because [pharmacists] can dispense salbutamol over the counter without a prescription, we have a responsibility to ask the right questions to determine patients’ level of control,’ she said. This could include asthma control tests. The Asthma Score is an example of such a test and comprises five questions. As part of this, pharmacists ask patients to rate their symptoms on a scale of one to five to indicate their asthma control over the last 4 weeks, including:
This could include asthma control tests. The Asthma Score is an example of such a test and comprises five questions. As part of this, pharmacists ask patients to rate their symptoms on a scale of one to five to indicate their asthma control over the last 4 weeks, including:
- How frequently are your symptoms preventing you from participating in work, school or play as well as normal?
- How often have you had shortness of breath?
- How often are your symptoms waking you up at night or earlier in the morning than usual?
- How often have you been using your reliever?
- How would you rate your asthma control?
‘If [salbutamol] has been [used] three or more times in the last week, that’s indicative of not having good asthma control,’ she said.
Promoting the right treatments
Over-the-counter short-acting beta agonists (SABAs) are associated with worse asthma outcomes, including death. But that isn’t because the medicine is harmful – it’s associated with inadequate asthma control, which has short and long term consequences.
Overall there is suboptimal use of inhaled preventers or inhaled corticosteroids, that have been shown to improve asthma control, reduce asthma exacerbations and reduce the risk of death from asthma. This includes suboptimal use of as-needed inhaled low-dose ICS/formoterol for people with mild asthma. This treatment is recommended by Australian and international guidelines as an effective alternative to regular maintenance ICS , in people with mild asthma – and is more effective and safer than using SABAs alone, said Ms Rigby.
 ‘This more flexible approach to treatment is ideally suited to people with mild asthma, many of whom are now at risk because they are not using an ICS preventer.’
‘This more flexible approach to treatment is ideally suited to people with mild asthma, many of whom are now at risk because they are not using an ICS preventer.’
Pharmacists should take the opportunity to provide some much-needed education to patients about the benefits of the budesonide/formoterol combination, said Ms Rigby.
‘Formoterol works just as well and quickly as salbutamol, but they’re also getting some inhaled corticosteroid – which helps with the inflammatory process going on in their lungs,’ she said. ‘Whereas with salbutamol, you’re just helping with the bronchoconstriction. It’s doing nothing about the underlying inflammation.’
When is a biologic appropriate?
When patients present with a prescription of prednisone, pharmacists can play an important role in appropriately identifying and informing them that this is a sign of poor asthma control and is a red flag that identifies a risk for severe acute asthma, including the risk of death, said Prof Wark.
Aspects to explore should include:
- Have they been prescribed a preventer?
- Are they using the preventer?
- Are they taking it appropriately?
- If they are taking their preventer appropriately but still experiencing acute asthma, they may be eligible for assessment by a specialist for a biologic agent
Asthma should be adequately controlled on moderate dose ICS together with a LABA. Persistence with high dose ICS or frequent courses of prednisone is certainly not the answer, said Prof Wark. A recent large population-based study conducted in the United Kingdom showed that stepping patients up to the highest doses of ICS adds little benefit to asthma management.
‘If a patient needs more than one or two courses of prednisone, and they’re on an ICS/LABA, you need to ask the question, “should they be receiving treatment with a biologic?”’ he said.
Prof Wark advises that patients who might benefit from a biologic include those:
- who continue to experience exacerbations and are overlying on prednisone
- with active type two inflammation, identified through blood counts and exhaled nitric oxide.
‘The impact prednisone has on health is enormous, it accumulates over a lifetime of exposure and we have very effective treatments for asthma that should reduce our reliance upon its use,’ he said. ‘People in regional and remote Australia, with poor asthma control appear to be at greater risk of needing to use prednisone.’
‘Up to 20% of people who present to a pharmacy for salbutamol haven’t had their asthma confirmed by spirometry.’
Debbie Rigby FPS
Once patients exceed a lifetime cumulative dose of 500 mg of prednisone, the health risks increase dramatically – leaving younger people who use the medicine particularly at risk.
‘Only one or two courses of prednisone in 12 months significantly increases the risk of developing osteoporosis, diabetes and infections such as pneumonia.’
Females over the age of 12 are at greater risk of poor asthma outcomes, said Prof Wark. When female patients have ongoing problems with asthma control and prednisone is needed – a biologic should be considered, he said.
‘If you’re not getting good asthma control, these alternative treatments work exceptionally well for everyone, including women.’
Get moving, and vaccinated
Vaccination can significantly reduce the impact of respiratory viruses among patients with asthma – particularly those aged 65 and over who may have other comorbidities.
Patients with asthma should receive:
- an annual influenza vaccination
- the pneumococcal vaccine
- a COVID-19 vaccine.
Pharmacists can also advise patients that influenza vaccines are free of charge for those with asthma, said Prof Wark.
‘RSV vaccines will soon be available, likely targeting patients aged 65 years and over.’
Asthma also interacts with other diseases – particularly diabetes and cardiovascular disease – with around three quarters of people with asthma having another chronic disease, said Prof Wark.
‘When you combine age and a number of comorbidities, there’s a more complex picture. Inactivity and obesity and the relationship to asthma, cardiovascular disease and chronic diseases such as diabetes – are all linked.’
Exercise and activity have been associated with improvements in asthma symptoms, along with overall asthma control.
While there should be ‘no limitations’ on the exercise patients with asthma can do, some factors might put them at risk.
‘For example, exercising in cold or dry air can increase your risk of bronchospasm,’ he said. ‘So warming up before exercise is advised.’
For more information, refer to PSA’s updated treatment guideline in the Australian Pharmaceutical Formulary and Handbook digital site.



 National Medicines Symposium 2024 speakers (L to R): Steve Waller, Professor Jennifer Martin, Professor Libby Roughead, Tegan Taylor[/caption]
National Medicines Symposium 2024 speakers (L to R): Steve Waller, Professor Jennifer Martin, Professor Libby Roughead, Tegan Taylor[/caption]


 This CPD activity is sponsored by Reckitt. All content is the true, accurate and independent opinion of the speakers and the views expressed are entirely their own.[/caption]
This CPD activity is sponsored by Reckitt. All content is the true, accurate and independent opinion of the speakers and the views expressed are entirely their own.[/caption]








