These oft-used medicines have become the analgesia of choice for many prescribers. But care should be taken before prescribing gabapentinoids to certain patients.
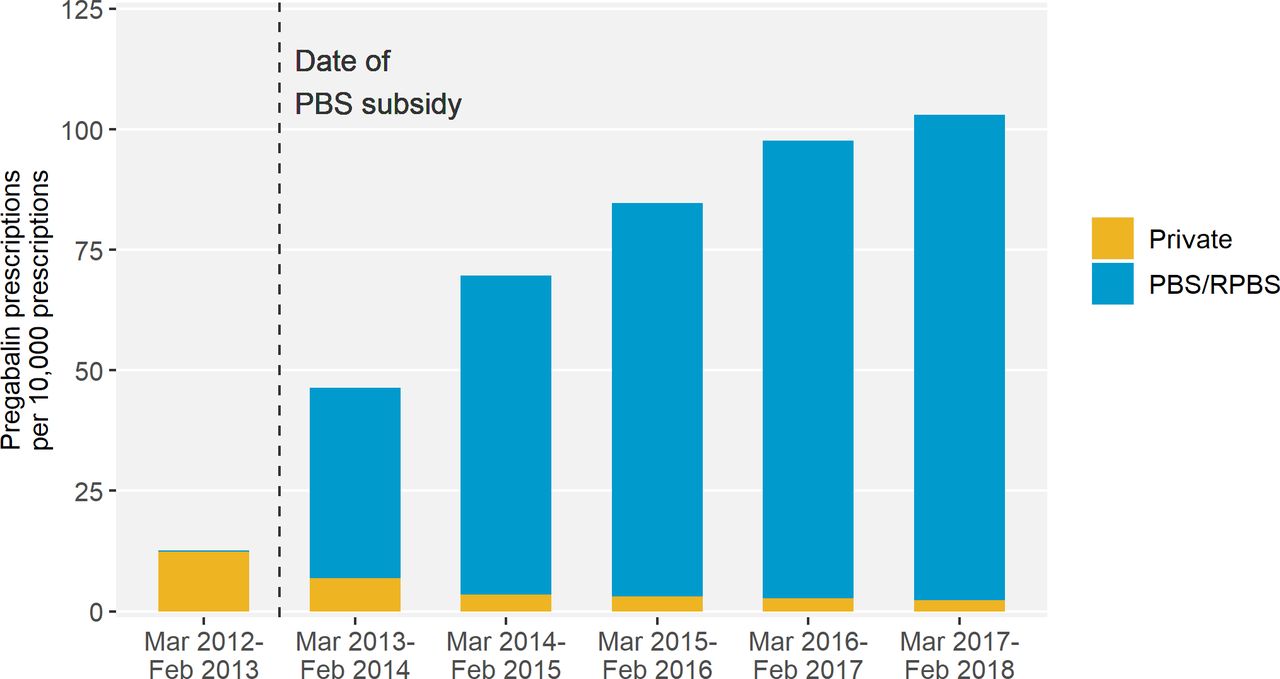
Gabapentinoid medicines are widely prescribed in Australia. Considered a safer alternative to opioids for neuropathic pain, there was an 8-fold increase in prescriptions for gabapentinoids from 2012 to 2018 – with 1 in 7 Australians aged 80 and older prescribed a gabapentinoid.
But a new study from Monash University researchers, including pharmacists Miriam Leung and Professor Simon Bell FPS, found that harm can be caused within 2 months of initiation.
Over a 5-year period, the researchers analysed data for 28,293 patients in Victoria who experienced hip fractures.
‘Our research found that patients who were recently dispensed either pregabalin or gabapentin had 30% higher odds of experiencing a hip fracture,’ Prof Bell told Australian Pharmacist.
Who is most at risk?
The link between gabapentinoid use and hip fractures existed across different age groups.
However, the risk of hip fracture associated with gabapentinoid medicines was highest in patients who were frail or had renal impairment, said Prof Bell.
‘Frail older people are prone to falls and fractures,’ he said. ‘One in 25 adults aged 80 years and older experience a hip fracture each year.’
The impact of these incidents can be fatal.
‘Around one in four people who experience a hip fracture die within 12 months,’ said Prof Bell.
How should pharmacists assess and manage falls risk?
For certain neuropathic pain conditions such as postherpetic neuralgia, diabetic neuropathy, and mixed or post-traumatic neuropathy, gabapentinoids such as pregabalin or gabapentin can provide effective relief.
However, while approved by the Australian Therapeutic Goods Administration for refractory focal (partial) epilepsy and neuropathic pain, gabapentin and pregabalin are often prescribed off label – with limited evidence to support efficacy for off-label indications.
In patients who are likely to see some benefit of therapy, pharmacists should advise patients how to minimise risk before dispensing these medicines.
‘The risk of falls is highest at the start of treatment,’ said Prof Bell.
‘Therefore, it’s important that pharmacists and other clinicians advise on strategies to minimise falls risk at this time. This could include avoidance of other falls-risk increasing substances such as alcohol.’
Evaluating what other medicines at-risk patients are prescribed is also an important strategy for preventing harm.
‘It’s known that gabapentinoids can cause side-effects such as drowsiness, sedation and dizziness,’ said Prof Bell.
‘These side-effects may increase the risk of falls, particularly if gabapentinoids are co-administrated with other psychotropic or cardiovascular falls risk medications.’
What impact can dose have on falls risk?
Given risk is highest at the outset of treatment, the starting dose of gabapentinoids can also have an impact on the likelihood of falls.
‘It’s advisable that patients start with a low dose and titrate slowly,’ said Prof Bell. ‘This particularly applies to people who are frail or have renal impairment.’
When is a discussion with the prescriber warranted?
The ongoing need for gabapentinoid treatment for neuropathic pain should be reviewed regularly, said Prof Bell.
‘If patients do not experience benefit after an adequate trial of treatment, then gradual discontinuation may be warranted,’ he said.
However, it’s important to advise people who take a gabapentinoid medicine that they shouldn’t stop taking their medication without first speaking with their prescriber or pharmacist first.
‘Stopping gabapentinoid medications abruptly can cause withdrawal symptoms,’ Prof Bell added.



 Jess Hadley, community pharmacist and Professional Officer at PDL[/caption]
Jess Hadley, community pharmacist and Professional Officer at PDL[/caption]
 Peter Guthrey, Senior Pharmacist – Strategic Policy at PSA[/caption]
Peter Guthrey, Senior Pharmacist – Strategic Policy at PSA[/caption]


 Professor Margie Danchin[/caption]
Professor Margie Danchin[/caption]

 Dr Peter Tenni[/caption]
Dr Peter Tenni[/caption]
 How should we deprescribe gabapentinoids, according to the Maudsley Deprescribing Guidelines[/caption]
How should we deprescribe gabapentinoids, according to the Maudsley Deprescribing Guidelines[/caption]






