Under a new government plan, pharmacists will be key to dramatically reducing HIV transmission.
Ahead of World AIDS Day (Sunday 1 December), the federal government released the Ninth National HIV Strategy (2024–2030) with the ambitious aim of eliminating HIV transmission by 2030.
Australia has achieved significant progress in reducing HIV transmission over the last decade, marked by a 33% decline in HIV notifications between 2014 and 2023.
Key to this success is increased rates of viral suppression among people living with HIV and the widespread uptake of pre-exposure prophylaxis (PrEP) among HIV-negative people, particularly among gay, bisexual, and other men who have sex with men.
Australia has also surpassed the Joint United Nations Programme on HIV/AIDS (UNAIDS) 2025 target of 86%, with 87% of all people living with HIV achieving viral suppression – reducing the risk of onward transmission to zero when there’s an undetectable viral load.
‘PSA is ready to work with government to investigate how pharmacists can be supported to increase HIV PrEP uptake to eligible people through pharmacist prescribing of PrEP, including long-acting injectables and oral formulations.’
a/prof FEI SIM FPS
‘In the 40 years since HIV/AIDS reached Australia, we have made remarkable progress,’ said Minister for Health and Aged Care Mark Butler. ‘This Strategy marks one of the final steps to achieving the virtual elimination of HIV transmission in Australia.’
We’ve come a long way
The first AIDS diagnosis in Australia occurred in 1982. But over the past four decades, Australia has experienced significant changes in HIV transmission rates.
Following the introduction of HIV testing in 1985, newly diagnosed HIV infections peaked at 2,773 cases in 1987. This dropped by 1,062 the following year and continued to decline to 833 in 1995.
By 1999, the number of new diagnoses had decreased significantly, largely due to the adoption of prevention practices such as safe sex and needle and syringe exchange programs. This downward trend continued into the 21st century, with 552 new HIV diagnoses reported in 2021, attributable to increased testing and widespread use of antiretroviral therapy.
Public perception has also shifted since the 1987 ‘Grim Reaper’ campaign, which aimed to raise awareness but instead instilled widespread fear, stigmatising affected communities.
Advancements in treatment transforming HIV into a manageable condition has led to a shift in public perception. But stigma remains an issue. In 2017, the Australian Survey of Social Attitudes revealed that 52% of the general public indicated they would still behave negatively towards people living with HIV.
Inequitable outcomes
Despite Australia’s successes, improvements in transmission rates have not been experienced across the board – with some populations and regions lagging in testing and PrEP uptake.
HIV diagnosis rates are disproportionately higher among individuals from culturally and linguistically diverse (CALD) backgrounds, with a 21.5% increase in HIV notifications over the past decade, with these patients often diagnosed late. Late diagnosis rates are particularly common among those born in Sub-Saharan Africa , Southeast Asia and Central/South America.
Among Aboriginal and Torres Strait Islander peoples, the HIV notification rate in 2022 was 3.2 per 100,000, compared to 2.2 per 100,000 in the non-Indigenous population.
What are the key aspects of the strategy?
The three key elements of the strategy include reducing new and late diagnoses, promoting understanding and support of U=U (Undetectable = Untransmittable), and implementing and sustaining models of service for intervention – particularly among priority populations.
How does the new national strategy compare to the previous one?
The Eighth National HIV Strategy (2018–2022) and Ninth National HIV Strategy share a commitment to reducing HIV transmission in Australia. But the goals and pathway to achieving this vary.
The Eighth Strategy aimed to meet UNAIDS 90-90-90 targets, focusing on increasing diagnosis, treatment, and viral suppression rates through prioritised expanded access to PrEP, post-exposure prophylaxis (PEP), and harm reduction programs. Addressing stigma and barriers to care for key populations, such as gay and bisexual men, sex workers, and Aboriginal and Torres Strait Islander peoples was also a key focus.
Key achievements under this strategy include allowing people living with HIV who are ineligible for Medicare to access free treatment through government-funded hospital pharmacies in 2023 and providing options for rapid HIV testing and self-test kits in pharmacies under updated Therapeutic Goods Administration regulations.
But the ninth iteration has pushed the envelope further towards virtually eradicating HIV transmission.
This strategy reflects advancements in treatment and prevention technologies, such as long-acting injectable antiretrovirals and expanded use of U=U.
With a higher proportion of men from CALD backgrounds and Aboriginal and Torres Strait Islander peoples acquiring HIV, the ninth strategy emphasises tailored approaches to improve access to care and ensure equitable treatment.
Multicultural organisations and Aboriginal Community Controlled Health Organisations are key to improving awareness of HIV in these communities. This includes design and delivery of culturally appropriate health promotion programs, delivery of peer-based services or directing patients to existing resources.
What’s the role of pharmacists?
Pharmacies are identified as a priority setting within the strategy as an important healthcare service used by priority populations to access HIV care, said a spokesperson for the Department of Health and Aged Care.
‘Pharmacists can play a key role in the virtual elimination of HIV transmission through the four key priorities of the strategy: prevention, testing, treatment and care, and stigma,’ said the spokesperson.
‘In partnership with the HIV sector, the Australian Government is investigating options to increase access to PrEP, including through pharmacists, as recommended by the HIV Taskforce and reflected in the new 9th National HIV Strategy.’
This includes options for promoting, prescribing or supplying PrEP through pharmacies, which is particularly vital among populations with limited access to healthcare services such as in rural or remote areas and CALD communities.
Simplifying PrEP regimen management, such as extending prescription cycles and monitoring requirements beyond 3 months and providing multiple pathology forms for repeat testing could encourage uptake.
However, at this time, there are no plans to change current access arrangements to post-exposure prophylaxis (PEP) for HIV, said the spokesperson.

While PSA shares the ambitious but achievable goal of the government’s updated national HIV strategy to virtually eliminate HIV transmission in Australia by 2030, PSA National President Associate Professor Fei Sim FPS said we can go further in utilising the skills and expertise of pharmacists to reduce barriers to care for people living with or at risk of HIV.
‘[This includes] making medications like PrEP and PEP more accessible to the communities who need them, increasing access to HIV testing and reducing stigma,’ she said.
‘PSA is ready to work with government to investigate how pharmacists can be supported to increase HIV PrEP uptake to eligible people through pharmacist prescribing of PrEP, including long-acting injectables and oral formulations.’
As new formulations come to the Australian market, such as long-acting injectable antiretroviral therapy, pharmacists can play an even greater role in supporting patients at risk of HIV, including both medicine administration and point of care testing.
‘To deliver on the goals of our HIV strategy, all health professionals, including pharmacists, need to do more to combat stigma,’ said A/Prof Sim. ‘This includes increasing awareness and understanding of U=U in the general population and supporting health workers to provide accessible, non-judgmental, and evidence-based care.’



 Rachel Neale from the QIMR Berghofer Medical Research Institute[/caption]
Rachel Neale from the QIMR Berghofer Medical Research Institute[/caption]



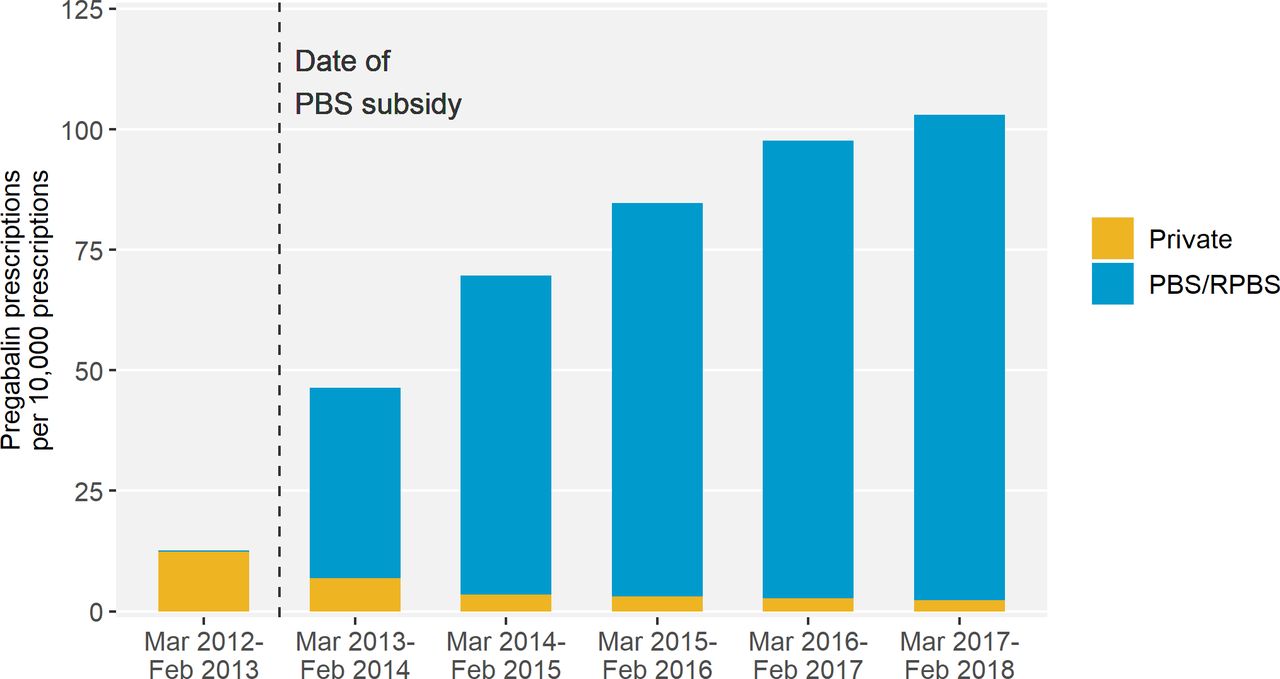 Source – Pregabalin prescribing patterns in Australian general practice, 2012–2018: a cross-sectional study[/caption]
Source – Pregabalin prescribing patterns in Australian general practice, 2012–2018: a cross-sectional study[/caption]

 National Medicines Symposium 2024 speakers (L to R): Steve Waller, Professor Jennifer Martin, Professor Libby Roughead, Tegan Taylor[/caption]
National Medicines Symposium 2024 speakers (L to R): Steve Waller, Professor Jennifer Martin, Professor Libby Roughead, Tegan Taylor[/caption]





