Data shows that while community pharmacists have smashed previous early-season influenza vaccination records, national coverage still lags dangerously.
Australia is experiencing its worst start to an influenza season, with case numbers surging and vaccination rates falling behind across key age groups.
Amid early peaks, a rise in influenza B cases, and sluggish immunisation uptake, Australian Pharmacist presents a visual snapshot of how the 2025 flu season is unfolding – and what must be done now to prevent a looming public health crisis.
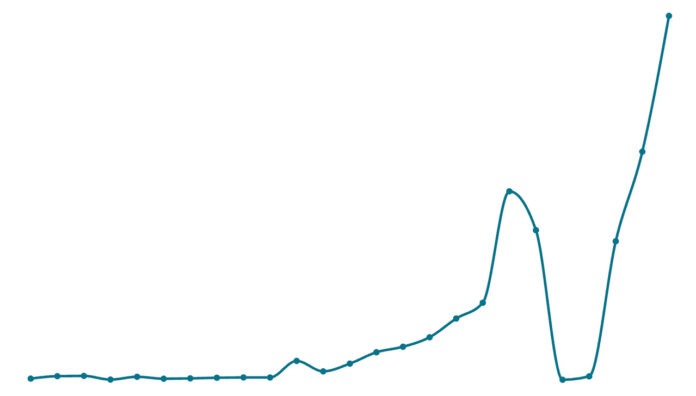
1. Influenza case numbers have reached unprecedented levels to start 2025
This year, influenza cases have reached their highest level in almost a quarter of a century (24 years). To date, there have been 58,203 notifications of laboratory-confirmed influenza reported to the National Notifiable Diseases Surveillance System (NNDSS) – with 2025 Quarter One case reports dwarfing that of previous years.
The flu season started earlier than usual this year, with cases surging sooner than in previous years. Early peaks often lead to higher overall case numbers – particularly when coupled with low immunisation rates.
In 2025, there has been a higher proportion of influenza B cases than in previous years, particularly in school-aged children and young adults, said Professor Anthony Lawler, Australian Government Chief Medical Officer. ‘Influenza B is often more common in children, and can result in more severe infections in children,’ he said.

With the northern hemisphere experiencing a severe influenza season, and strains in this region typically migrating south, Rural Doctors Association of Victoria president Louise Manning said the trend was ‘worrying’.
‘We’re quite concerned that, given the severity of symptoms and the number of hospitalisations in the northern hemisphere in their winter, that we’ll have a similar picture here,’ Dr Manning told the ABC.
2. Pharmacists have had a fast start to influenza vaccination
Data over the last 4 years shows pharmacist-administered vaccines are experiencing continued growth.
Key factors influencing this growth include increased trust in the pharmacy profession to administer vaccines as well as accessibility. With longer operating hours – including evenings and weekends – pharmacies offer greater accessibility, allowing patients to receive influenza vaccinations without appointments or extended wait times. This convenience factor makes pharmacy a more flexible alternative to traditional healthcare settings such as General Practice.
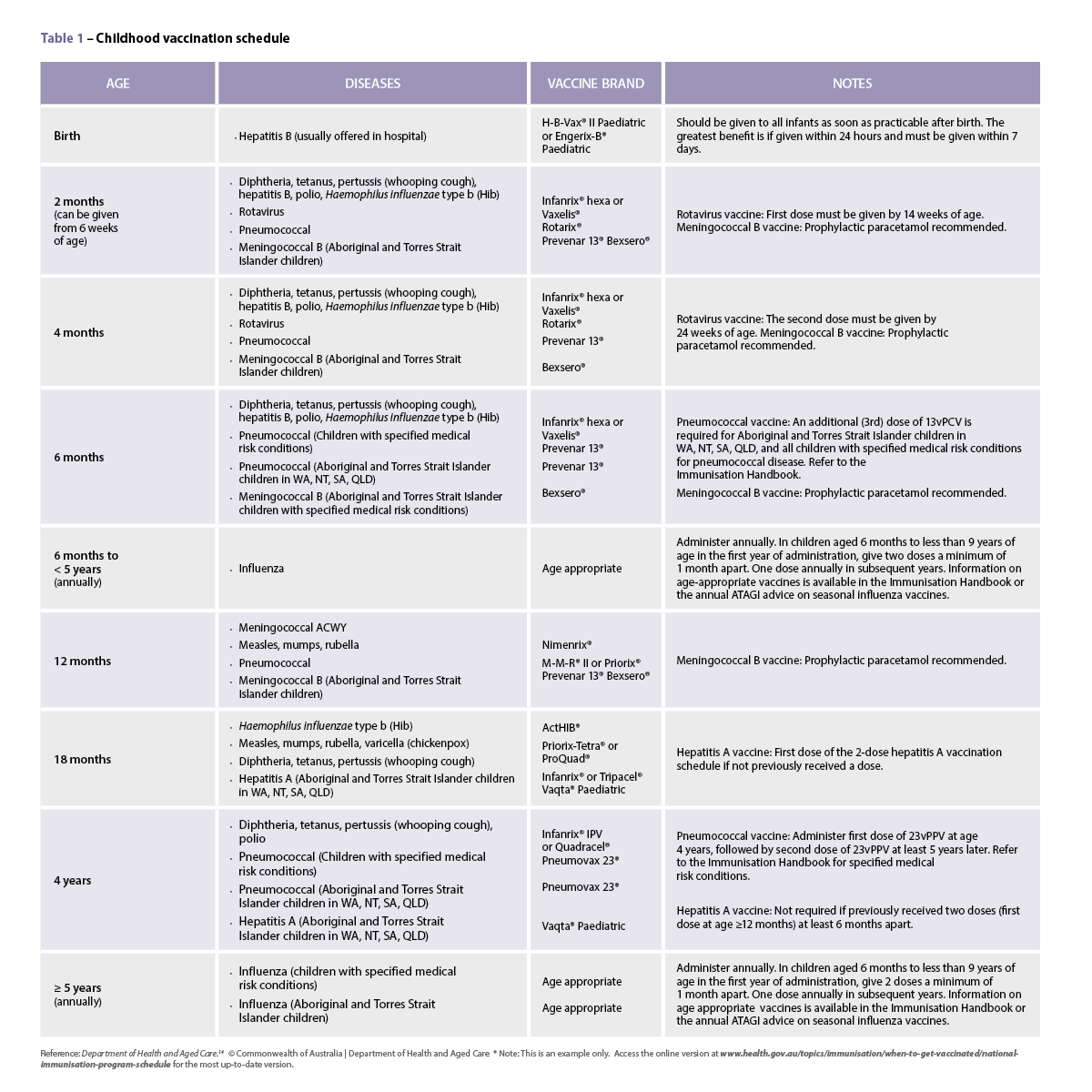
3. Vaccination rates are far too low in children under 5
When it comes to influenza, children aged 0–5 are one of the most vulnerable cohorts – with the high risk of severe complications sometimes leading to hospitalisations, often due to pneumonia, and death.
Despite the risks, vaccination rates remain low in this age cohort, with only 7,398 children aged 0–5 receiving the influenza vaccine so far this year.
Despite the influenza vaccine being covered under the National Immunisation Program for this age group, less than half (45%) of parents are aware that their child can be vaccinated free of charge.
In 2024, only 25.8% of children 6 months to 4 years received an influenza vaccine – with three quarters of this at risk population remaining unvaccinated.
Many parents believe that influenza is not a serious disease or that the vaccine is ineffective or unsafe, with 29% exposed to misinformation and 26% influenced by anti-vaccine sentiment through social media.
Vaccine access can also prove challenging. To boost participation in young children, PSA maintains that there should be ‘no wrong door’ when it comes to vaccination – meaning pharmacists should be able to provide influenza vaccines alongside other childhood immunisations, said Chris Campbell MPS, PSA General Manager Policy and Program Delivery.
‘What [this] does do is increase the convenience for someone to be able to get the vaccine at a time and place of their choosing,’ he said.
‘There should be an increase in vaccine uptake in children under 5 years of age when there’s an opportunity for an entire family to come to the pharmacy and get vaccinated.’
4. Vaccination rates in all cohorts need to improve to stave off a devastating influenza season
The latest data on influenza vaccination coverage in Australia for 2025 reveals concerningly low uptake across all age groups and jurisdictions. Western Australia, Tasmania, and Victoria report particularly low figures at this stage among children 6 months to >5 years and aged 5 to under 15 years, with some states showing uptake as low as 0.1%.
Among patients aged 50 to under 65 years, national coverage sits at 2.8%, with Queensland (4.5%) and South Australia (4.0%) leading the charge. Coverage increases more significantly in the over 65s demographic – with South Australia (14.2%) and Queensland (12.6%) again topping vaccination coverage.
Vaccine manufacturers are also expecting a surge in cases, with CSLSeqirus revealing it has boosted its vaccine output by 100,000 doses this season.
To protect the community from a particularly nasty influenza season, experts have urged people to roll up their sleeves and get vaccinated.
‘If you don’t want to get crook get vaccinated,’ Public Health Association of Australia chief executive Terry Slevin said.
‘You’re less likely to get crook and if you do get crook, you’ll be crook for a shorter period of time … and reduce the misery.’



 This CPD activity is supported by an unrestricted education grant by Reckitt.[/caption]
This CPD activity is supported by an unrestricted education grant by Reckitt.[/caption]
 Case scenario
Case scenario





 Jess Hadley, community pharmacist and Professional Officer at PDL[/caption]
Jess Hadley, community pharmacist and Professional Officer at PDL[/caption]
 Peter Guthrey, Senior Pharmacist – Strategic Policy at PSA[/caption]
Peter Guthrey, Senior Pharmacist – Strategic Policy at PSA[/caption]