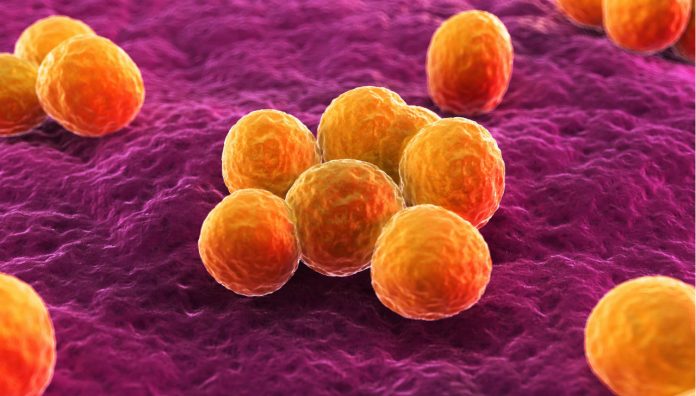
There has been an increase in incidents of community-associated Staphylococcus aureus bloodstream infections (CA-SABs) in Victoria and Western Australia (WA). Pharmacists have a role to play in infection control and prevention.
A study, which surveyed 10,320 hospital-reported S. aureus bacteraemia (SAB) cases in Victoria and WA from 2011-2016, found that 6,800 cases were community-associated (CA), as opposed to healthcare-associated, with the number of CA-SABs increasing by eight and six per cent per year in Victoria and WA respectively.1 Methicillin-susceptible S.aureus (MSSA) was the cause of most CA-SABs.
Importantly, patients 60 years and over had higher incidences of CA-SABs, with men twice as likely to acquire the infection than women of the same age.
The study comes in response to hospital reports received by the Victorian Healthcare Associated Infection Surveillance System (VICNISS) and Healthcare Infection Surveillance Western Australia (HISWA) in 2016 and 2017, informing them of increased incidences of CA-SABs.
These increases may be due to virulent S. aureus strains or changes in host risk factors.1 Aged care facility residents may be at particular risk as infections in this group would have been classified as CA-SABs in the study.
Pharmacists’ role in infection control and prevention
According to Naomi Weier, Project Pharmacist at the Pharmaceutical Society of Australia (PSA), ‘pharmacists have a key role to play in counselling patients on infection control and prevention’.
‘This includes counselling patients on hygiene measures such as covering sores or wounds and correct use of dressings, counselling and promotion of the importance of correct handwashing techniques and washing hands regularly and providing education and advice on exclusion periods for infectious conditions if required,’ she said.
According to health.vic The incubation period is most commonly 4–10 days, although this can vary. Transmission is usually via direct or indirect contact with a person who has a discharging wound or clinical infection (e.g. respiratory or urinary tract), or who is colonised with S.aureus (e.g. approximately 50% of the population). Infection control and prevention is required for as long as the lesions are purulent and continue to drain or carrier state continues.
Weier also sees an opportunity for pharmacists to ‘educate patients with risk factors (e.g. immunocompromised patients etc.) for certain infections on symptoms to look out for and strategies for reducing the risk of infection’.
Recognising infection in patients
S. aureus is most commonly responsible for skin infections and will likely present with redness, swelling, pain, heat and pus-filled lesions such as boils and abscesses.2
However, S. aureus can also infect joints, bones, blood, the gastrointestinal tract and other major organs, with symptoms varying based on the infection’s location in the body.
Sepsis, symptoms include rapid breathing, an elevated heart rate, fever, chills and disorientation.3
Dangers of infection
While boils and abscesses are often relatively mild infections and can be easily treated with drainage and appropriate antibiotics, invasive S. aureus infections can be more difficult to treat and can often be life-threatening. In fact, S. aureus bacteremia has an in-hospital mortality of 20-30%, a 2018 review reported.2,4
S. aureus can cause complications such as endocarditis (infection and inflammation of the heart’s inner lining) and septic thrombophlebitis (clot/venous thrombus). Increased microbial load and a decrease in the body’s ability to fight the infection, if left unchecked, can lead to organ failure.4
Sources of infection should always be identified to decrease rates of mortality. Persistent fever should be monitored and blood cultures sampled.4
Further complications arise when patients have methicillin-resistant S. aureus (MRSA), as the bacteria will not be susceptible to the penicillins normally used to treat MSSA. Instead, patients will need to be identified as soon as possible and treated with the appropriate antibiotic(s) (e.g. vancomycin, teicoplanin, daptomycin etc.) in order to clear the infection.4 Further information can be found in eTG and AMH.
Referring patients to seek medical help
According to Weier, ‘pharmacists should refer patients presenting with symptoms of bacterial infection requiring antibiotics to their doctor immediately,’ while also taking the opportunity to explain the role of antibiotics, knowing what to expect and when they should be used. Repeat prescriptions for an antibiotic should only be dispensed after clarifying clinical appropriateness, in line with PSA’s Choosing Wisely Recommendations.
‘Also, when presented with a prescription for an antibiotic, pharmacists should review the prescription to assess its appropriateness for the patient – including the correct antibiotic, dose, directions, and duration – and counsel patients on the role of antibiotics and their correct use,’ she said.
This is in line with the International Pharmaceutical Federation’s views, suggesting that the pharmacist’s role is to encourage responsible use of antibiotics to achieve optimal patient outcomes and prevent antibiotic resistance.5
Finally, ‘pharmacists should refer patients back to their doctor if there is no improvement or if symptoms worsen’, Weier explained.
-
- Imam N, Tempone S, Armstrong P, et al. Increased incidence of community-associated Staphylococcus aureus bloodstream infections in Victoria and Western Australia, 2011-2016, 2019. The Medical Journal of Australia. At: https://www.mja.com.au/journal/2019/210/2/increased-incidence-community-associated-staphylococcus-aureus-bloodstream
- Staphylococcus aureus infection, Queensland Government. 2017. At: http://conditions.health.qld.gov.au/HealthCondition/condition/14/33/132/staphylococcus-aureus-infection
- Staph infections: What you should know, Penn Medicine. 2018. At: https://www.pennmedicine.org/updates/blogs/health-and-wellness/2018/may/staph-infections
- Jung N, Rieg S. Essentials in the management of S. aureus bloodstream infection. 2018. Infection. At: https://www.ncbi.nlm.nih.gov/pubmed/29512028
- Fighting antimicrobial resistance, International Pharmaceutical Federation. 2015. At: https://www.fip.org/files/fip/publications/2015-11-Fighting-antimicrobial-resistance.pdf



 Dr Peter Tenni[/caption]
Dr Peter Tenni[/caption]
 How should we deprescribe gabapentinoids, according to the Maudsley Deprescribing Guidelines[/caption]
How should we deprescribe gabapentinoids, according to the Maudsley Deprescribing Guidelines[/caption]



 Pharmacists have always prescribed, but they have the potential to prescribe much more
Pharmacists have always prescribed, but they have the potential to prescribe much more