Around 2.1 million Australians are affected by osteoarthritis (OA), with the knees a commonly affected area. With the condition more prevalent in those over 45 years of age, and Australia’s population continuing to age, the number of people living with knee OA skyrocketed by 126% between 1990 and 2019.
Given Australia is also in the midst of an obesity epidemic, and the risk of OA doubling among those who are overweight – these numbers are only set to increase.
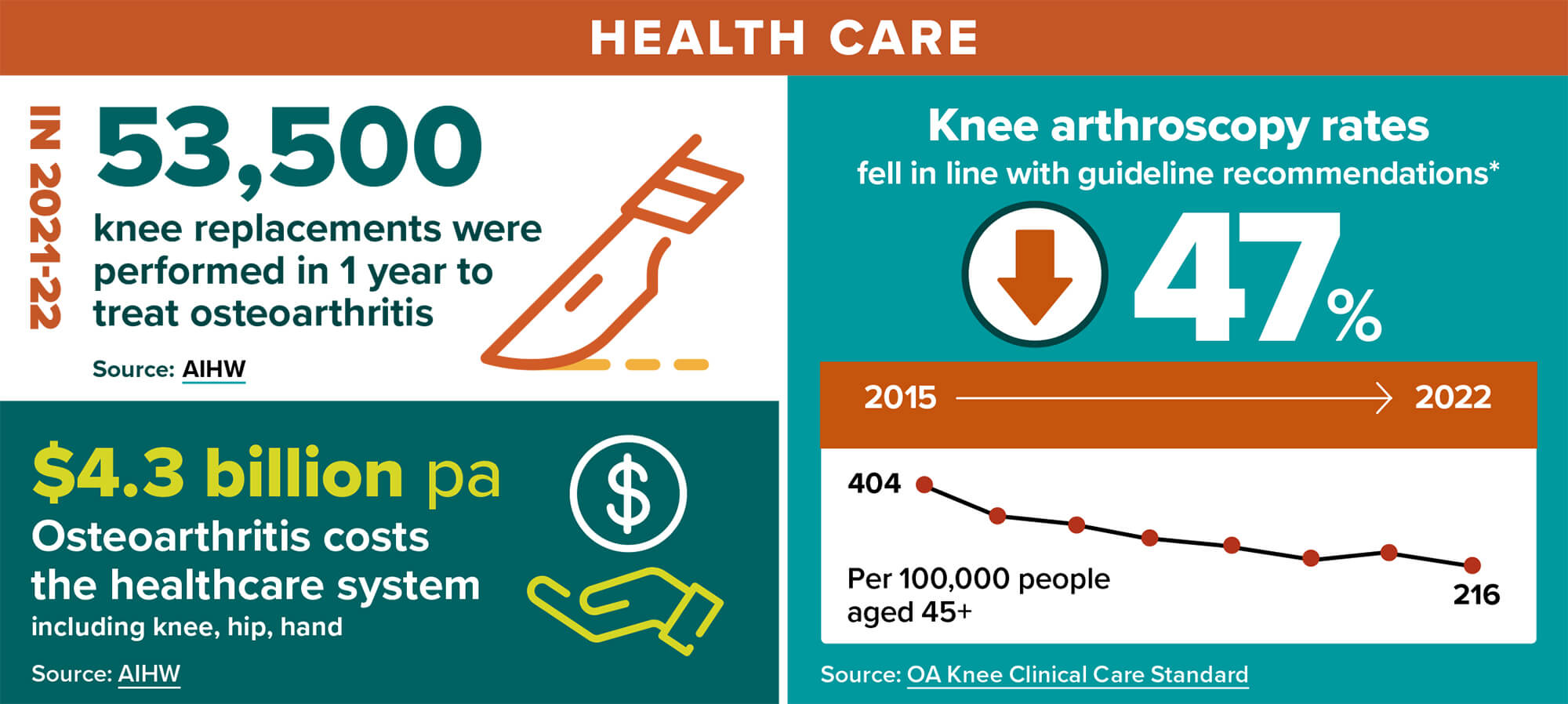
While surgery is often seen as an unavoidable solution to OA pain, the Australian Commission on Safety and Quality in Health Care has suggested a new approach.
In its revised 2024 Osteoarthritis of the Knee Clinical Care Standard, the Commission recommends a focus on non-surgical approaches and community and primary healthcare management – in line with the latest evidence.
Pharmacists are therefore integral to knee OA management, with a primary role in providing counselling around medicines used for pain, said GP and Medical Advisor for the Commission, Dr Phoebe Holdenson Kimura.

‘People need to be supported throughout their knee OA care journey in the community – whether through their physio, pharmacist or GP,’ she said.
Australian Pharmacist looks at some of the key shifts in the Standard that impact pharmacists.
Lifestyle interventions are first line
As outlined in the Standard, Dr Holdenson Kimura said a diagnosis of knee OA can confidently be given based on just the patient’s history and an examination.
‘Evidence shows there’s a poor correlation between imaging reports and pain and functional impairment,’ she said. ‘In the case of an atypical presentation of knee pain that is suspected OA, an X-Ray would be the imaging of first preference rather than a CT scan or an MRI.’
 When reports don’t mention knee OA, this can lead people down another pathway of thinking there’s a meniscal or cartilage problem that can be fixed with surgery, said Dr Holdenson Kimura.
When reports don’t mention knee OA, this can lead people down another pathway of thinking there’s a meniscal or cartilage problem that can be fixed with surgery, said Dr Holdenson Kimura.
‘But we know that for people who are over 45 years of age, there’s no role for arthroscopic intervention in uncomplicated knee osteoarthritis.’
From the beginning of the care journey, if people engage in activities such as exercise or weight management, they might be able to put off surgery or not need it at all, said Dr Holdenson Kimura.
‘Joints are designed to be loaded, meaning they are nourished with movement, which is both safe and beneficial for people living with knee OA.’
Dr Phoebe Holdenson Kimura
The Standard also emphasises the importance of creating an individualised management plan with patients who have knee OA, which includes understanding:
- their pain level
- how the pain impacts their life
- preferences for exercise and movement.
‘I have some patients who love aqua aerobics or walking in the pool, and others who say, “that definitely would not work for me”,’ she said. ‘So we need to work with people, because the exercise they enjoy is what they are going to persist with.’
Conversations with a physiotherapist or exercise physiologist can lead to a comprehensive physical assessment and exercises to strengthen particular muscle groups, and look at the biomechanical process going on within the entire limb.
‘Pharmacists can check in with how patients are progressing with their goals, and communicate any changes they’ve noticed with the rest of the team,’ said Dr Holdenson Kimura.
While there’s ‘good evidence’ that 5–10% weight loss can lead to improvements to both pain and function for people living with knee OA, weight loss is not an easy journey.
‘These conversations need to be had in a sensitive way, and we need to work with people’s needs and preferences rather than providing blanket statements and expectations around weight loss,’ she said.
Changes in medicines used to manage pain
Since the first publication of the Standard in 2017, Dr Holdenson Kimura said evidence has mounted that most injectable medicines for knee OA are not effective.
 ‘The revised Standard provides a recommendation against the use of intra-articular injections of platelet rich plasma and hyaluronic acid because there’s not good evidence that they provide any benefit while also carrying a significant expense for the patient,’ she said.
‘The revised Standard provides a recommendation against the use of intra-articular injections of platelet rich plasma and hyaluronic acid because there’s not good evidence that they provide any benefit while also carrying a significant expense for the patient,’ she said.
‘Like surgery, people might see those injections as a silver bullet,’ said Dr Holdenson Kimura. ‘But unfortunately, the evidence just isn’t there.’
Corticosteroid injections in the knee can be used as a short-term treatment for pain relief. However, repeated injections can lead to a risk of cartilage damage or further joint deterioration.
The new Standard also contains a strong recommendation against the use of opioids for knee OA, with the risks outweighing any potential benefits.
‘As a practising GP, if a pharmacist contacts me to say, “I’ve noticed this patient has been using this opioid for quite some time and they’ve told me it’s for their knee OA, and I wanted to discuss whether you think that’s still appropriate for the patient”, I’d be really receptive to having that conversation,’ said Dr Holdenson Kimura.
‘But there are some situations, such as if the person is awaiting surgery, that it could be appropriate.’
In terms of over-the-counter analgesics that can be used for pain associated with knee OA, non-steroidal anti-inflammatory drugs (NSAIDs) are first-line pharmacological treatment following an assessment of the risks.
When a patient is having a flare, NSAIDs play a role in managing those flares, she said. ‘But NSAIDs, particularly in older people, have a number of adverse effects, so it’s important to use at the lowest effective dose for the shortest time possible in people without absolute contraindications.’
Topical NSAIDs or capsaicin as an adjunct to other treatment strategies can also have a role, and can help with self-management.
While less effective than NSAIDs, paracetamol can also be considered for patients at risk of harm from NSAID use, such as those with risk factors for gastrointestinal, kidney or cardiovascular toxicity.
However, complementary medicines such as glucosamine, chondroitin and turmeric, often used for knee OA, should not be recommended, said Dr Holdenson Kimura.
‘Unfortunately, there is not good quality evidence for the use of those medicines for knee OA pain,’ she added.
Getting the right message across
Throughout the quality statements in the Standard, there are communication tips to ensure healthcare professionals, including pharmacists, communicate messages about knee OA in a unified and empathetic manner that empowers patients.
‘We need to change the way we talk about knee OA,’ said Dr Holdenson Kimura.
‘People are being told it’s “wear and tear, bone on bone, and degenerative” which leaves them in a passive position where they think the more they walk on it, the more damage it’s causing.
‘Joints are designed to be loaded, meaning they are nourished with movement, which is both safe and beneficial for people living with knee OA.’
A key message for pharmacists to impart is that medicines are there to help people with knee OA to mobilise their joints – rather than remove their pain all together.
‘The message we want to encourage is that medicines can help to reduce pain so that you can exercise and do your usual activities,’ she said Dr Holdenson Kimura. ‘But they shouldn’t replace doing exercises to strengthen your knees or losing any excess weight.’



 Professor Margie Danchin[/caption]
Professor Margie Danchin[/caption]

 Dr Peter Tenni[/caption]
Dr Peter Tenni[/caption]
 How should we deprescribe gabapentinoids, according to the Maudsley Deprescribing Guidelines[/caption]
How should we deprescribe gabapentinoids, according to the Maudsley Deprescribing Guidelines[/caption]



 Pharmacists have always prescribed, but they have the potential to prescribe much more
Pharmacists have always prescribed, but they have the potential to prescribe much more




