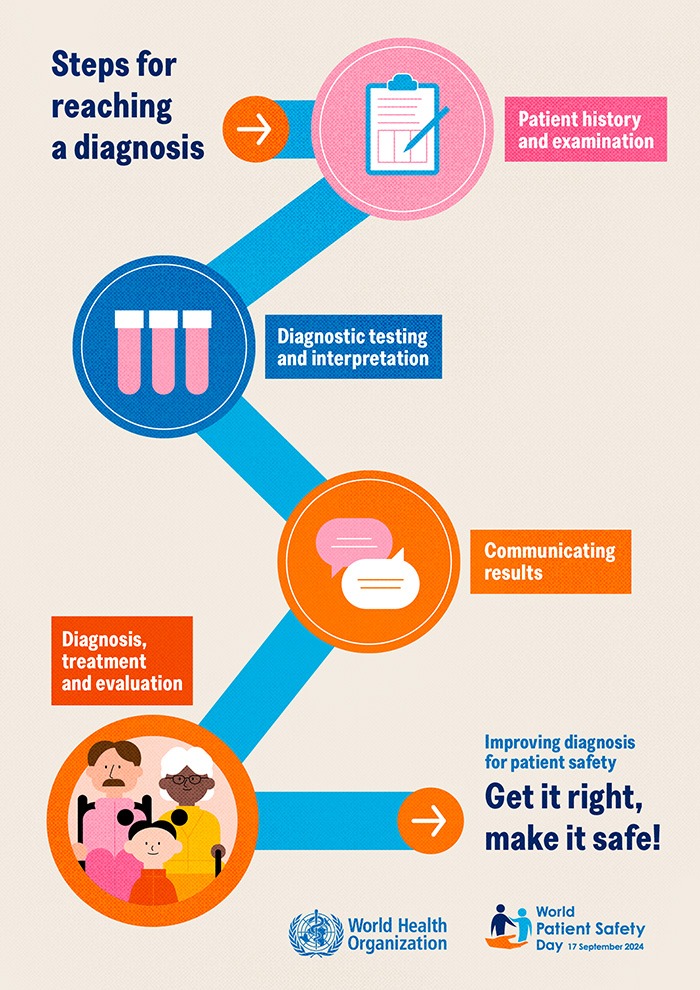
It was World Patient Safety Day on 17 September, with this year’s theme around improving diagnosis for patient safety.
Australian Pharmacist examines three health conditions where diagnosis is commonly delayed, incorrect, or missed – and pharmacists’ important role in ensuring an accurate and timely diagnosis to improve treatment outcomes.
 COPD is significantly underdiagnosed
COPD is significantly underdiagnosed
Around 50% of people living with Chronic Obstructive Pulmonary Disorder (COPD) are estimated to be undiagnosed.
While patient symptoms and a physical examination can support diagnosis, full spirometry is required to diagnose the condition correctly, said Advanced Practice Pharmacist Associate Professor Debbie Rigby FPS, head of PSA’s Respiratory Care Community of Specialty Interest.

‘There are many other respiratory conditions that can present as symptoms of COPD such as wheeze, shortness of breath, chest tightness, chronic cough and poor exercise intolerance – including asthma,’ she said.
An additional layer of complexity is the stigma associated with COPD, which is commonly perceived as a disease solely caused by cigarette smoking.
‘However, we know that around 30% of people diagnosed with COPD have never smoked a cigarette,’ said A/Prof Rigby. ‘There are many other factors, including genetic [predisposition] and environmental exposures that can lead to COPD.’
Because of the high rate of underdiagnosis of COPD, the condition is often undertreated.
‘It’s important to appropriately treat COPD, because although it can’t be cured, we can slow the progression in decline in lung function with medications as well as non-pharmacological treatments such as pulmonary rehab,’ she said.
The Lung Foundation Australia’s Lung Health Checklist can help pharmacists identify people who are at risk for COPD, looking at factors such as:
- cigarette smoking history
- exposure to environmental and workplace substances such as dust or fumes.
Pharmacists can also conduct case finding or screening via handheld devices such as a COPD-6 or a PIKO-6.
‘These screening tools measure the ratio of FEV1/FEV6, which is the forced expiratory volume in 1 second over the forced expiratory volume in 6 seconds,’ said A/Prof Rigby. ‘They can identify people who would then be referred to their GP for spirometry.’
There is under-use of spirometry in general practice, confounded by the COVID-19 pandemic, during which there was a reluctance to conduct the test due to the potential of spreading the virus through aerosolisation.
To help bridge this gap, A/Prof Rigby said appropriately trained pharmacists can also perform spirometry.
While spirometers do provide some degree of interpretation when presenting results, diagnosis requires further interpretation, said A/Prof Rigby.
‘The definition of FEV1/FVC of less than the lower limit of normal or 0.7, which is the criteria measured by the machine,’ she said. ‘But other factors in addition to that ratio need to be considered for diagnosis and for determining treatment.’
The Lung Foundation’s COPD-X Handbook indicates that first line therapy for confirmed COPD is a long-acting muscarinic antagonist (LAMA) or long-acting beta2 agonist (LABA). A LAMA/LABA combination product can be considered if appropriate.
‘With asthma, all adults and adolescents should be on an inhaled corticosteroid (ICS), perhaps with the addition of a LABA,’ she said. ‘So if a patient with COPD was incorrectly diagnosed with asthma and placed on an ICS/LABA, they could have an increased risk of pneumonia [due to the ICS].’
There are also medicine indicators that could signal that patients have undiagnosed COPD, including coming into the pharmacy for over-the-counter SABA due to shortness of breath, or for cough medicines due to chronic cough.
‘Pharmacists should take a patient history, including whether they have smoked cigarettes, or are still smoking, and should refer them for review with their GP, said A/Prof Rigby.
There is also emerging evidence on the harm of vaping as a COPD risk factor.
‘For patients coming into the pharmacy after 1 October for Schedule 3 vaping products, pharmacists have a real opportunity to have those conversations whereby we could identify if they have one or more risk factors for COPD,’ she said.
Endometriosis can take almost a decade to diagnose
Endometriosis is often dismissed as period pain or misdiagnosed due to overlapping symptoms such as pelvic pain, irritable bowel issues or fatigue, said Nicolette Ellis MPS, Chair of Chronic Pain Australia.

‘The National Pain Report 2024 highlights that while it takes an average of 3 years to diagnose a chronic pain condition, endometriosis typically takes 7–9 years to diagnose,’ she said.
‘This delay is largely due to a lack of education, awareness, and the fact that it can only be definitively diagnosed through invasive laparoscopy.’
However, timely diagnosis is crucial for managing pain and preventing its escalation.
‘Early detection improves outcomes, reducing the physical and emotional toll on patients,’ said Ms Ellis. ‘Delayed diagnosis often leads to feelings of dismissal, with many told the pain is “all in their head,” further worsening the vicious cycle of chronic pain.’
Pharmacists should be aware that endometriosis can present with a wide range of symptoms, including:
- stomach distension
- pain during ovulation
- vaginal sensitivity
- lower back pain
- symptoms resembling irritable bowel syndrome
- repeated but ineffective pain management (e.g. tramadol prescriptions).
‘It’s important to ask patients about their symptom history and patterns, while also considering other pelvic pain conditions that often coexist with endometriosis,’ she said.
When pharmacists suspect a patient has endometriosis, Ms Ellis said they should:
- Ask about timing and patterns of pain (e.g. not just during menstruation)
- Enquire about heaviness of bleeding and severity of pain.
- Look for signs such as
-
-
-
- back or abdominal pain
- bloating and stomach distension
- Pain during bowel movements or sex
- Excessive use of heat packs
- Days missed from work or school due to pain
- Impact on daily function, mood, and overall well-being
-
-
-
- Ask about menstrual irregularities
- Investigate family history of endometriosis or related conditions.
- Refer the patient for further evaluation with a GP or specialist.
Pharmacists can also help patients navigate the health system by:
- providing information about local healthcare resources and specialists with expertise in pain management
- recommending specialist pelvic pain clinics in primary care settings to reduce wait times and facilitate access to multidisciplinary care.
- suggesting consumer resources such as Chronic Pain Australia and Endometriosis Australia, which offer valuable support and guidance for navigating healthcare and managing conditions.
Children’s chronic pain is often overlooked
Children’s chronic pain, frequently misattributed to growing pains, takes an average of 3 years to diagnose, said Ms Ellis.
‘The healthcare system is significantly under-resourced, with only six paediatric pain clinics nationwide, yet the prevalence of chronic pain in children is similar to that in adults (1 in 5),’ she said.
Conditions such as juvenile arthritis, migraines, complex regional pain syndrome and functional abdominal pain are common in children.
‘They may report persistent pain, tiredness, or emotional distress,’ said Ms Ellis. ‘Pharmacists should ask about the duration of the pain, other symptoms, any triggers, and how it affects daily activities, as well as encourage parents to keep track of these patterns.’
Pharmacists should be concerned if pain in children persists beyond 3 months, as this could indicate a chronic pain condition.
While service provision for paediatric pain can be challenging, pharmacists should recommend consulting with a GP as the first step, and if needed, refer to paediatricians or pain specialists, she said.
Referrals to doctors with innovative approaches to easing children’s anxiety around medical appointments can help, for example this Darwin Doctor has a therapy turtle on hand to make repeated appointments bearable for young patients, some of whom have rheumatoid arthritis.
‘Pharmacists can direct parents to resources such as Chronic Pain Australia’s Kids in Pain campaign, running from 23–29 September for additional support and guidance, Ms Ellis added.
For more information, pharmacists can refer to the following PSA resources:
- Essential CPE: Chronic obstructive pulmonary disease (COPD)
- CPD: How to talk about smoking cessation in priority populations
- APF treatment guideline: Salbutamol and terbutaline for bronchospasm.



 Jess Hadley, community pharmacist and Professional Officer at PDL[/caption]
Jess Hadley, community pharmacist and Professional Officer at PDL[/caption]
 Peter Guthrey, Senior Pharmacist – Strategic Policy at PSA[/caption]
Peter Guthrey, Senior Pharmacist – Strategic Policy at PSA[/caption]


 Professor Margie Danchin[/caption]
Professor Margie Danchin[/caption]

 Dr Peter Tenni[/caption]
Dr Peter Tenni[/caption]
 How should we deprescribe gabapentinoids, according to the Maudsley Deprescribing Guidelines[/caption]
How should we deprescribe gabapentinoids, according to the Maudsley Deprescribing Guidelines[/caption]






