After much media scrutiny, the federal Department of Health and Aged Care has announced a ban on compounded Glucagon-like peptide-1 receptor agonists (GLP-1RAs) such as semaglutide and tirzepatide.
The ban follows advice from the Therapeutic Goods Administration (TGA), after a Consultation to remove GLP-1RAs from the pharmacist extemporaneous compounding exemption, and a high-profile raid on a Melbourne compounding pharmacy earlier this year.
Here’s what pharmacists need to know.
What are the reasons for the ban?
The government has expressed concerns that compounded GLP-1RAs are not identical to TGA-approved products – such as Ozempic and Mounjaro – and are not clinically evaluated by the TGA for safety or efficacy.
There are also concerns that the ‘replica’ medicines are being produced and supplied on a ‘commercial-like scale’ that is not in line with quality standards.
This is refuted by telehealth start-up Eucalyptus, which said that none of its patients reported unexpected serious adverse outcomes in the 6 months it has been selling compounded Ozempic.
When does it come into effect?
The ban on compounded GLP-1RAs will be introduced on 1 October 2024, giving patients and prescribers 4 months to consider a new management plan.
What does the ban mean for patients?
The government has estimated that 20,000 patients are using compounded GLP-1RAs, predominantly for off-label weight loss use. However, recognising low visibility of the volume of compounded GLP-1RAs being supplied, the government has acknowledged uncertainty about the number of patients who use these medicines.
Someplace the number significantly higher, with NIB-owned online script service Midnight Health purporting to have 10,000 patients who use compounded Mounjaro alone.
‘We think about 70,000 people use compounded weight loss medications,’ said NIB CEO Mark Fitzgibbon.
This means tens of thousands of patients, and their prescribers, will need to plan for alternative therapy.
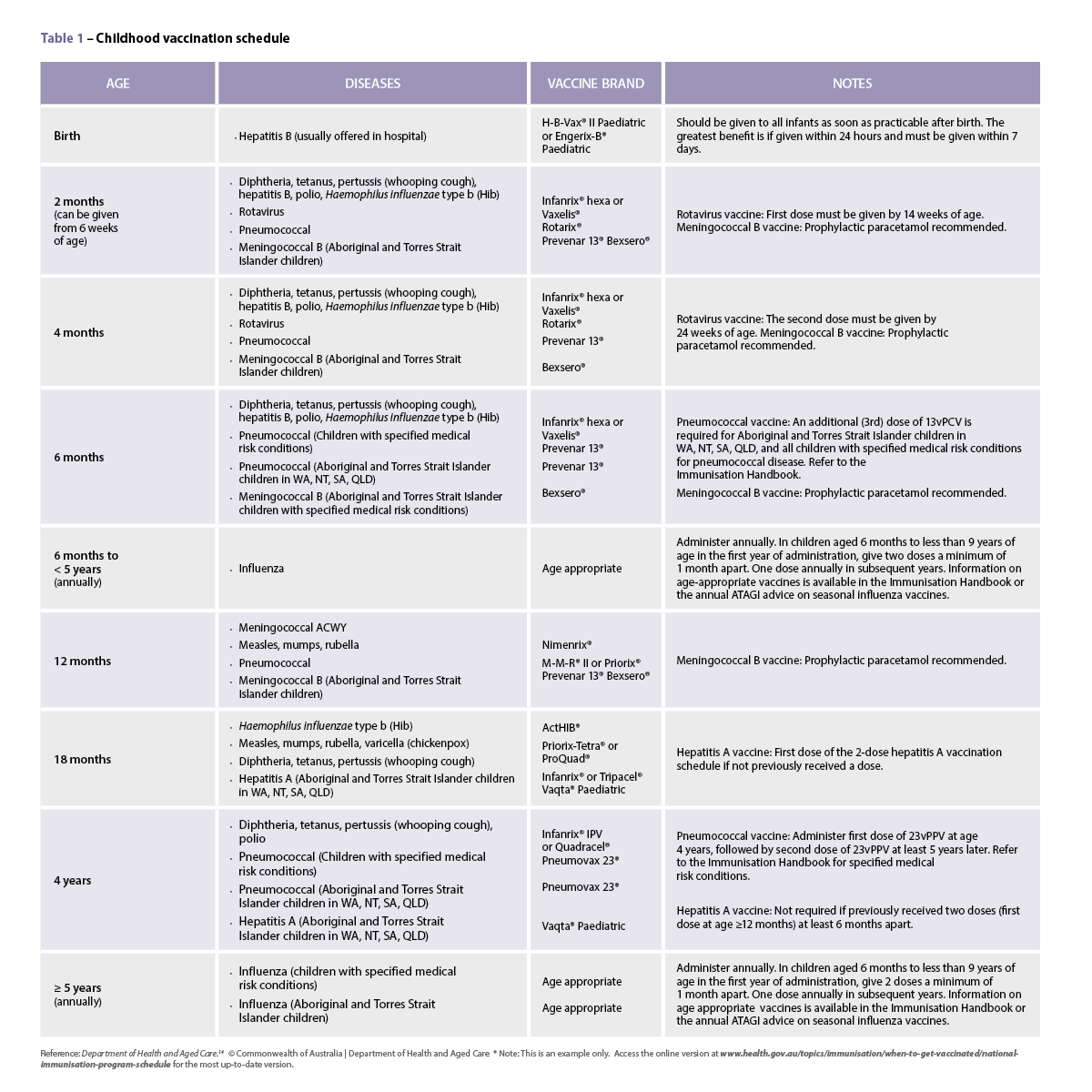
Stock of the following GLP-1RAs approved by the TGA are expected to be replenished on:
- tirzepatide (Mounjaro): 31 August 2024
- dulaglutide (Trulicity): 31 December 2024.
A spokesperson for Novo Nordisk told Australian Pharmacist that ‘there will be continued, limited intermittent availability in Australia of Ozempic until December 2024’ due to ongoing ‘unprecedented strong demand’.
Prescribers have been advised not to initiate new patients on Ozempic for type 2 diabetes, unless there are no suitable alternative treatments or there is an urgent clinical need.
Pharmacists should limit supplies of semaglutide to those stabilised on the treatment. The PBAC recommended a shift from streamlined authority to phone authority for patients initiated on Ozempic, however this has not yet come into force.
Liraglutide (Saxenda) – a GLP-1RA approved by the TGA to be used as a weight loss treatment – is not currently in short supply. Wegovy, an alternative brand of semaglutide approved by the TGA for weight management, is not currently available in Australia. With demand of the medicine outstripping supply, there may be no stock of Wegovy available until next year.
What do patient groups think?
The Consumers Health Forum of Australia (CHF) said it was concerned about the safety and quality of compounded GLP-1RAs after issues were raised in the media. But its position is that patients in need should still be able to access the compounded medicine.
‘What we have been hearing from consumers for a very long time now, is that there is absolutely a supply issue which is impacting those people who legitimately need it,’ said CHF CEO Dr Elizabeth Deveny.
Patients using compounded Ozempic are concerned they will no longer be able to source a medicine that they have considerably benefitted from.
‘[The compounded drug] made me not feel guilty about using it, and taking away the pens from people who should take first priority [is deeply disappointing],’ said one patient.
‘This is a medication I’ve relied on to get to a point where I’m happy with myself … It will cause distress and anxiety for a group that gets so much benefit from it.’
However, this has not been a universal, as detailed on Four Corners recently.
What about pharmacists?
Compounding pharmacist Ganesh Tumkur, who owns Berwick Springs Pharmacy in Victoria said he doesn’t compound GLP-1RAs in his pharmacy but is concerned that the way the issue has been announced and portrayed ‘implants a bit of mistrust in pharmacists’.
Mr Tumkur also took issue with the compounding of medicines being mischaracterised as a ‘loophole’ rather than a ‘gap filler’ when manufacturers are unable to meet consumer demand.’
Compounding is a long-standing clinical competency of pharmacy practice, giving patients access to medicines where there is a gap in commercial product suitability or availability. It is a necessary practice to support the health and wellbeing of Australians.
Compounding should only occur where appropriate standards of safety and quality can be met. As the peak body for pharmacists, PSA produces guidance for pharmacists on how to achieve this.
The compounding of sterile formulations, including all injections, can only be safely done in sophisticated sterile suite facilities which meet high standards for product integrity and avoiding contamination.
PSA recognises the TGA’s concerns that there have been cases of high-volume of semaglutide compounding which are alleged to have fallen well short of these expected standards. PSA recognises the government’s announcement as a pragmatic measure to manage risks associated with these alleged rouge operators.
What’s next in terms of medicines for weight loss?
A new drug will soon be trialled in Melbourne for patients who are overweight or who have type 2 diabetes. CagriSema, which is a combination of Ozempic active ingredient and another appetite suppressant, has shown promising results.
‘In previous trials of a smaller number of people we’ve seen this approach where you combine the two drugs together, (it) is more effective than just using Ozempic alone,’ said Royal Melbourne Hospital endocrinologist, Associate Professor John Wentworth.
‘Everyone in the study is expected to lose weight and to have their diabetes improve.’


 Professor Anthony Lawler, Australian Government Chief Medical Officer,
Professor Anthony Lawler, Australian Government Chief Medical Officer, 
 This CPD activity is supported by an unrestricted education grant by Reckitt.[/caption]
This CPD activity is supported by an unrestricted education grant by Reckitt.[/caption]
 Case scenario
Case scenario




 Jess Hadley, community pharmacist and Professional Officer at PDL[/caption]
Jess Hadley, community pharmacist and Professional Officer at PDL[/caption]
 Peter Guthrey, Senior Pharmacist – Strategic Policy at PSA[/caption]
Peter Guthrey, Senior Pharmacist – Strategic Policy at PSA[/caption]







