With the right knowledge, pharmacists can help heal patients’ acute wounds and injuries — and grow a gaping area of practice.
Whether it’s spending time at the beach or in the bush, cooling off in the pool, hosting a barbecue or playing backyard cricket, there’s a lot to love about summer in Australia. But with more people outside getting active or enjoying themselves on holiday, it can also be a time when acute injuries such as cuts, burns, strains and sprains present themselves.
Community pharmacists have long been destinations for patients seeking treatment for minor injuries. While the management of acute wounds is within the scope of practice of all registered pharmacists in Australia,1 the role has become more specialised in recent years, with increasing numbers of pharmacists training in wound care and establishing wound care clinics. In Queensland, a pilot program even allows participating pharmacists to prescribe for acute wound management, among other conditions.2

Accredited pharmacist and member of PSA’s WA Branch Committee Lusi Sheehan MPS has a postgraduate qualification in wound care and runs courses for pharmacy teams. As the most accessible healthcare professionals, she says pharmacists can have a profound impact on a patient’s outcomes and quality of healing.
‘If someone gets a cut, graze or skin tear, they are often able to see us on the day it happens, instead of waiting to see a doctor, which could take weeks. That’s really essential to prevent complications,’ she says.
According to Wounds Australia, more than 420,000 Australians experience chronic wounds each year, costing the nation’s health and aged care budgets more than $3 billion annually. On top of this, each patient with a chronic wound spends about $4,000 out of pocket.3 As all chronic wounds begin as acute wounds, Ms Sheehan says pharmacist intervention can save time and money, both for patients and the healthcare system.
‘Chronic wounds are very costly. But if pharmacists can see a patient quickly and prevent their injury from becoming chronic, then it can significantly reduce the burden on the patient, as well as the government.’
The whole patient
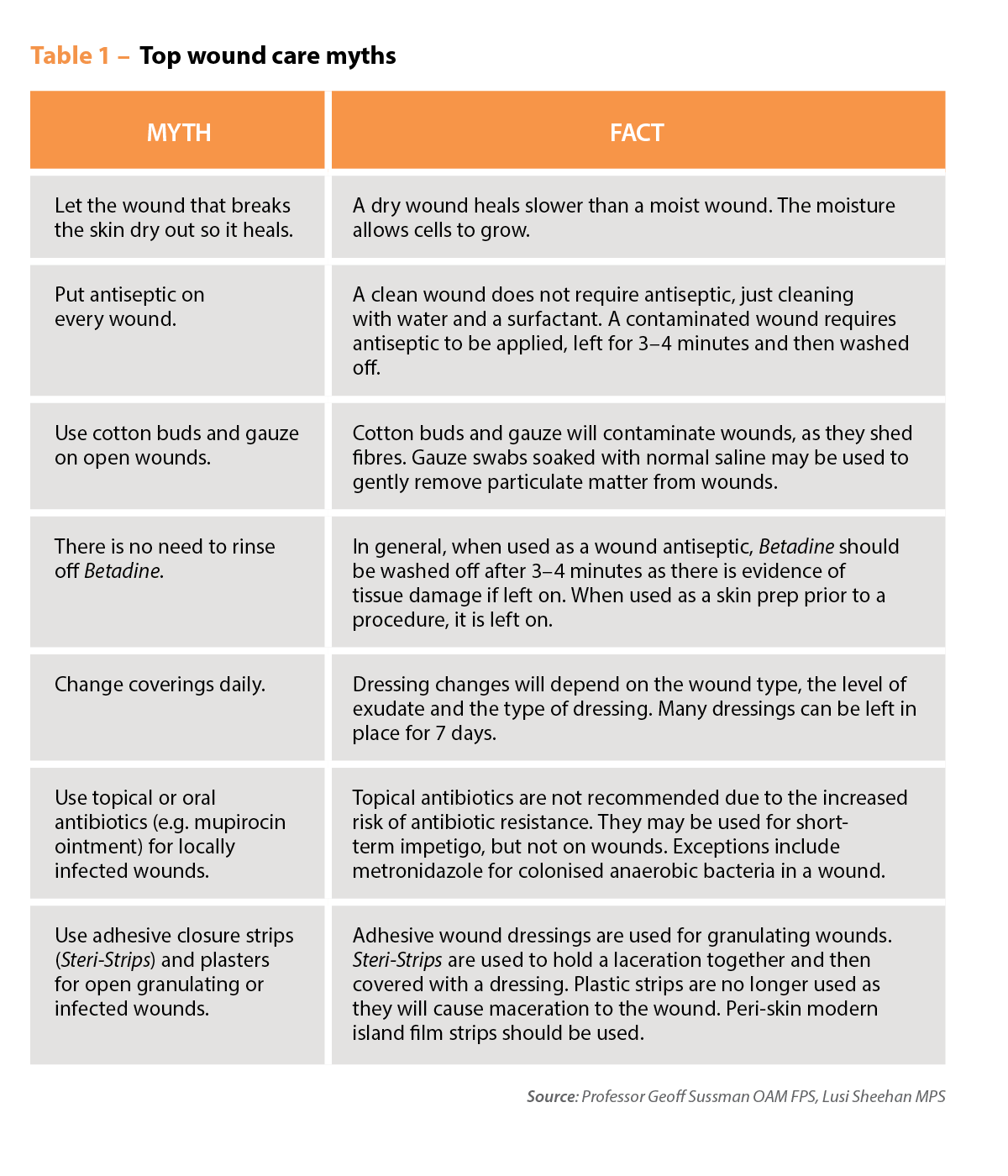
Cuts, abrasions, burns, skin tears, strains and sprains are the acute injuries pharmacists are most likely to encounter. It is important to know which can be managed with the right knowledge and training, and when it is appropriate to refer. The first step is to assess any injury, including asking the patient how long they have had it, what caused it and what (if anything) they have used on it, Ms Sheehan says.
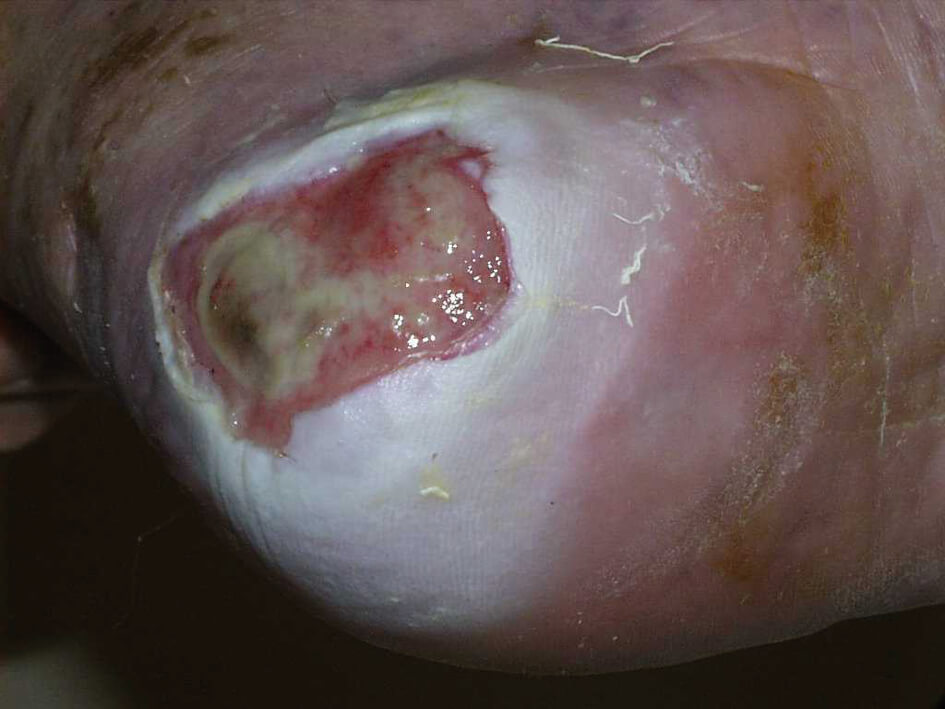
‘If it’s a wound, the best thing is to ask if you can have a look at it, because a patient might describe something that looks completely different to what it actually is,’ she says. ‘You need to assess the wound bed, determine the aetiology of the wound and look for any signs of local or systemic infection.’ (See the CPD: ‘Wound infections: identification, prevention and management’ for more information on infection.)

Professor Geoff Sussman OAM FPS helped to establish wound care as a speciality in Australia after seeking out best practice approaches from around the world. Ultimately, he says it is about ‘treating the whole of the patient, not the hole in the patient’.
‘It is vital that you obtain a full health history to identify any comorbidities or medication that may delay healing,’ Prof Sussman says. This means considering all factors that might affect healing, including a patient’s age, any medical conditions, obesity, nutritional status, genetic factors, current medicines and lifestyle, such as smoking and excessive alcohol consumption.
Pharmacists should also take antimicrobial stewardship into account when managing wounds, Prof Sussman says. ‘Most wounds don’t need antibiotics. Antiseptic, yes, but not antibiotics. This is important, as research has shown an overuse of antimicrobials in wound care.’
‘Ultimately, it is about treating the whole of the patient, not the hole in the patient.’
Professor Geoff Sussman OAM FPS
It is also important for pharmacists to collaborate with other healthcare professionals to get the best outcomes for their patients, he says. ‘Pharmacists can play an important role in community wound management, but they can’t do it alone. You should also know your limitations and when to refer. You should have a list of local wound specialists, podiatrists, dermatologists, etc, for this purpose.’
In the management of some wounds, when to refer will depend on an individual pharmacist’s knowledge and training, says Claire Antrobus MPS, PSA Manager – Practice Support.
‘A pharmacist who has done additional training in wound management is well placed to handle many acute wound presentations,’ she says. ‘However, if a wound is, or is at risk of becoming, clinically infected – such as partial or full thickness burns – or if the patient has an increased risk of wound infection, the patient may need to be referred for further assessment.
‘Some medicines and some medical conditions can affect wound healing, and referral may be necessary, for example, if a patient is on corticosteroids or has diabetes. Other potential reasons for referral include severe pain or chronic or non-healing wounds.’
Taking stock
Prof Sussman authored the Wound Management chapter of the Australian Pharmaceutical Formulary and Handbook (APF), available online or the 26th edition hard copy due for release in February 2024. It provides an overview of wound management and dressing selection, based on the type of wound a patient presents with. As there are so many products on the market, he says it is vital that pharmacists have the right stock.
‘Pharmacists should look at their product range and ensure it is updated regularly. This doesn’t mean getting in extra stock, but replacing out-of-date products, such as gauze, crepe, plastic strips and most adhesive tapes, with modern products.’
Kerri Barwick MPS, PSA’s General Manager of Education, Training and Knowledge Development, agrees it is crucial that pharmacies stock the right consumables. ‘Once a pharmacist has been well trained in wound care, it becomes apparent that the common recommendation of an island dressing is often not adequate. The full range of dressings, from hydrocolloid to alginate and foam dressings, can go a long way to better treat wounds.

‘I recommend pharmacists review Section 10 of the APF, which has an excellent section on wounds as a great starting point, covering principles of wound dressing selection, a comprehensive list of different dressings available and descriptions with pictures of different wounds.’
More specialised wound consumables can be very expensive, Ms Barwick says. In future, she would like to see a subsidy for patients who find it difficult to afford them. ‘This should be coupled with a payment for pharmacists for the consultation. Some wounds only require a short consultation, with treatment and recommendations that are quite straightforward, but there are complex wound management scenarios that need longer consultation, follow-up and review.’
A new area of expertise
Pharmacies are in the ‘perfect position’ to become destinations for wound care, Ms Barwick says, provided pharmacists have the correct training, products and set-up.
‘Pharmacists have an opportunity to train in a new area. As a trusted profession that is accessible and available, we can use this position, as well as the consult area most pharmacies already have, to make this service available.
‘The right training and the right products lead to better patient care, and there is a great opportunity for a pharmacy to become a destination for this. A review of the consultation area to ensure it is an appropriate size with impervious floors, a metal trolley for dressings and implements, a daybed and handwashing facilities would need to occur before a clinic could begin.’
There are many ways to upskill, with wound care training programs ranging from continuing professional development to postgraduate qualifications.
‘When thinking about upskilling in wound management, some of the things pharmacists should consider include how wound management fits within their current scope of practice, community needs and other local healthcare providers that offer wound management services,’ Ms Antrobus says. ‘They can then tailor their education accordingly.’
According to Ms Sheehan, there are ‘lots of benefits’ to pharmacists upskilling in wound care.
‘For pharmacy owners, it is a valuable service because it drives patients to your pharmacy by providing something innovative that might not be available everywhere. The same can be said for stocking a range of dressings that are evidence-based and are probably quite different from other pharmacies or GP clinics, who can’t always stock a good range of dressings. And the dressings they do have often don’t heal wounds very well.
‘Patients get access to a prompt wound care service that can help prevent an acute wound from becoming chronic, saving them money, as well as the burden of having to be hospitalised if the wound isn’t healing well.
‘And as a pharmacist, I find it really interesting to see the difference wound treatment can make and to see the changes as a wound heals,’ says Ms Sheehan. ‘I find it really rewarding as a career pathway, using my clinical skills but also patient communication skills and collaborating with other health professionals. Patients are usually very, very grateful when you’re able to help them heal their wound.’
References
- Sheehan L, Dias S, Joseph M, et al. Primary care wound clinics: a qualitative descriptive study of patient experiences in community pharmacies. Pharmacy (Basel) 2022;10(4):99.
- Queensland Health. North Queensland Community Pharmacy Pilot. 2023. At: health.qld.gov.au/__data/assets/pdf_file/0028/1207990/NQPP-Pharmacist-Info.pdf
- Wounds Australia. Pre-budget submission to fight Australia’s chronic wound epidemic. 2022. At: treasury.gov.au/sites/default/files/2022-03/258735_wounds_australia.pdf
- Sansom LN, ed. Australian pharmaceutical formulary and handbook [online]. Canberra: Pharmaceutical Society of Australia; 2023.




 Categorisation of heart failure
Categorisation of heart failure A focus on SGLT2is
A focus on SGLT2is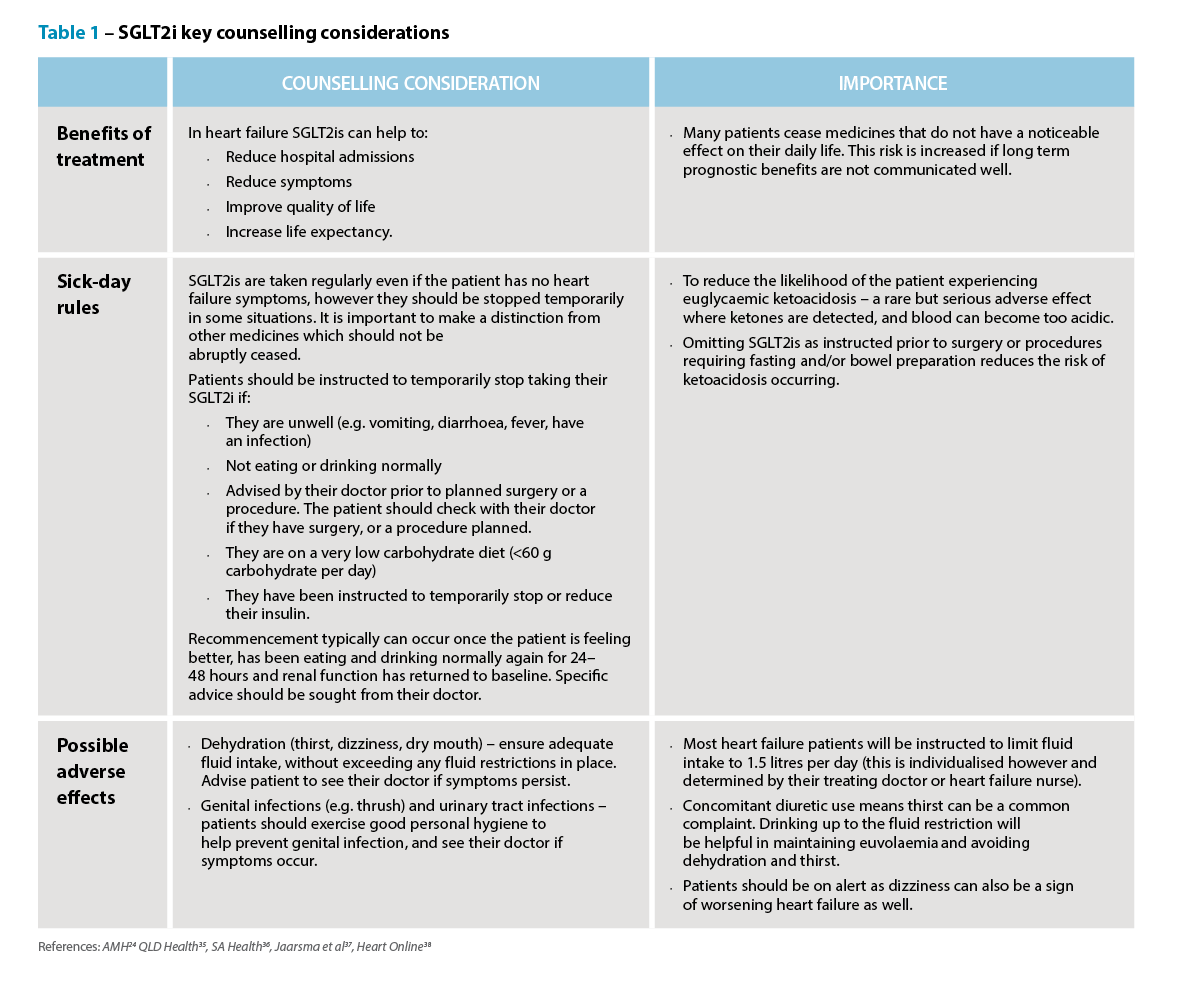 Knowledge to practice
Knowledge to practice 
 Professor Anthony Lawler, Australian Government Chief Medical Officer,
Professor Anthony Lawler, Australian Government Chief Medical Officer, 
 This CPD activity is supported by an unrestricted education grant by Reckitt.[/caption]
This CPD activity is supported by an unrestricted education grant by Reckitt.[/caption]
 Case scenario
Case scenario









