A new cautionary advisory label (CAL D) for antibiotics that will replace decades of advice to take the medicines ‘until all used’ or ‘until all taken’ will be released next year.
Details about the revised CAL D are being released to coincide with World Antimicrobial Awareness Week (18–24 November), ahead of the CAL being included in the digital version and next print edition of the Australian Pharmaceutical Formulary (APF25), to be published in January 2021.
Key points:
|
Completion of a recommended course of therapy with an antibiotic can improve therapeutic outcomes and reduce the incidence of relapse. However, taking antibiotics for longer than necessary does not improve outcomes and increases the risk of acquiring resistant bacterial strains.
‘The new label is a significant change to previous recommendations around the duration of treatment for antibiotics and is the result of various stakeholders coming together to help combat bacterial resistance to antibiotics,’ a spokesperson for PSA’s APF team told Australian Pharmacist.
‘Pharmacists should be aware that the required duration of treatment may require a smaller quantity of antibiotic than the pack size supplied to the patient.’
Practice changes
As the label represents a shift in what patients are used to, pharmacists need to educate patients about the appropriate duration of treatment and bacterial resistance to antibiotics, the APF spokesperson said.
If a patient is not aware of the prescribed duration of treatment and it is not specified on the prescription, the pharmacist should contact the prescriber to confirm the duration.
‘[It is important to] counsel patients appropriately about the exact duration of treatment and safe disposal of any unused antibiotics in the dispensed pack,’ the spokesperson said.
Patients should be advised never to keep unused antibiotics. They should also be informed that it is not safe or environmentally friendly to flush unused medicines down the toilet or drain, or throw them in the general rubbish. Disposal in this way can lead to growth of resistant bacteria in these environments.
Under the new instruction, patients should stop taking the antibiotic when the prescribed duration of treatment is complete.
‘Pharmacists should also advise the patient to contact the prescriber if their symptoms worsen or do not improve in the timeframe advised by the prescriber,’ the spokesperson said.
Antimicrobial use awareness
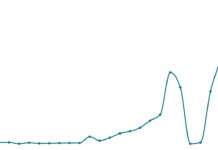
According to the Antimicrobial Medicines Dispensing from 2013–14 to 2017–18 report, released last month, antimicrobial medicines use in Australia declined from 2013 to 2018, but the country’s rate remains high by OECD standards.
The report also revealed a sustained pattern of high use in 22 hot spots in some of the most disadvantaged areas of major cities, including outer areas of Sydney, Brisbane and Melbourne.
This contrasts with ‘encouraging’ results showing a fall of 13.3% nationally, the report stated.
In 2017–18, 28.2 million prescriptions for antimicrobials were dispensed in the community, compared with 30.3 million prescriptions in 2013–14, the report from the Australian Commission on Safety and Quality in Health Care found.
It is the first study to analyse antimicrobial prescribing at every level: national, state and territory, Primary Health Network (PHN) and local area.
The commission’s Senior Medical Advisor Professor John Turnidge said being able to compare data would enable the healthcare sector to develop more targeted strategies to tackle the threat of antimicrobial resistance.
‘It is significant that we are witnessing the first evidence of a consistent decline in antimicrobial consumption in Australia since the last decline in 2003,’ he said.
‘We are moving in the right direction but have more work to do, as the volume of antimicrobial use is still more than double that of comparable OECD countries.’
The issue of antimicrobial resistance was addressed in the federal budget, with a $22.5 million investment in antimicrobial usage and antimicrobial resistance surveillance, to monitor and address the threat.


 Professor Anthony Lawler, Australian Government Chief Medical Officer,
Professor Anthony Lawler, Australian Government Chief Medical Officer, 
 This CPD activity is supported by an unrestricted education grant by Reckitt.[/caption]
This CPD activity is supported by an unrestricted education grant by Reckitt.[/caption]






 Jess Hadley, community pharmacist and Professional Officer at PDL[/caption]
Jess Hadley, community pharmacist and Professional Officer at PDL[/caption]
 Peter Guthrey, Senior Pharmacist – Strategic Policy at PSA[/caption]
Peter Guthrey, Senior Pharmacist – Strategic Policy at PSA[/caption]







