Accurate, clear and concise note taking can save careers. But what is the best format for your notes?
Pharmacists often don’t think to make notes because they are too busy. Or they don’t think an interaction is worthy of recording. Or they assume others will make records or notes in a suitable manner. Some don’t have, or are not aware of, a suitable means to make records in their dispensing systems.
None of these scenarios is a surprise to Gary West MPS, a former community pharmacist with 35 years in the profession and who works at Pharmaceutical Defence Limited (PDL), which provides professional indemnity insurance for pharmacists.
‘In my 8 years of work as a Professional Officer at PDL I have had many cases where a lack of suitable or sufficient records has impacted on a patient and/or pharmacist.’
This may occur when changes to medicine therapies are communicated verbally but not accurately recorded in a suitable manner.
It’s also happened, he says, in cases where allegations are made against a pharmacist for their advice or practice and the pharmacist may have little to no recall of advice given or events that transpired to effectively defend their actions.
Similarly, he says, problems can loom when a pharmacist may choose to delay or decline supply having concerns with the prescribed or requested treatment and a patient makes allegations of discrimination, unprofessional practice or makes a vexatious claim against the pharmacist.
Logically, notes should be professional in their content, Mr West stresses. Pharmacists should write them knowing they may be read and interpreted by other health professionals, regulatory agencies including the Pharmacy Board of Australia and lawyers, in cases of legal action.
A subject line, such as ‘UTI consult and med supply’ might be suitable if the pharmacist provided a treatment for an uncomplicated urinary tract infection.
If, after discussing with a patient that a referral to a GP was needed, for example, they should not just say verbally ‘you’d better go and see a doctor about that’.
Instead Mr West advises a more professional approach that should be adopted by more in the profession. ‘Generate a written referral. “Dear Dr X. I’ve spoken with our mutual patient today and after discussions I’m concerned that these symptoms have been reported and warrant further review. I’d be grateful if you’d see the patient and also provide me with some feedback”.’
A record of that referral saved somewhere suitable in whatever software system that is used by the pharmacy would be ideal, Mr West advises.
It’s likely, he says, that software will emerge in the near future to assist pharmacists to better record information with a good note-taking facility for different interactions.
 It’s a need for the profession as expansion of scope activities occur and also, as patients become more aware of privacy and security entitlements, we are seeing more complaints, according to Mr West. ‘The better and more frequent the note-taking is, the less likelihood of consequence for a pharmacist if there has been a complaint made.
It’s a need for the profession as expansion of scope activities occur and also, as patients become more aware of privacy and security entitlements, we are seeing more complaints, according to Mr West. ‘The better and more frequent the note-taking is, the less likelihood of consequence for a pharmacist if there has been a complaint made.
‘We are becoming more focused on both the recognition that pharmacists are engaging in a therapeutic relationship with patients – with these expanded scope activities – and they may not recognise that because of that therapeutic relationship the onus of responsibility to have more professional and appropriate records is greater.’ So always take notes.
On duty 24 hours a day on a rolling roster, PDL professional officers hear about lots of less-than-ideal interactions in which notes should have been taken and stored.
Dose administration aid changes given verbally by patients or prescribers, decisions to defer or decline supply, discussions with prescribers about pharmacists’ concerns for safety and wellbeing of a patient and treating expanded scope activities as “business as usual” without appropriate levels of records for hormonal contraception supply and resupply, for instance, are not good practice, Mr West points out.
While not practical to record hundreds of daily interactions by pharmacists, he says they do need to trust their gut feelings that a patient might escalate a matter and to realise the benefits of taking notes especially in situations around staged supply or Real Time Prescription Monitoring medicine supply. Once a complaint is made to a regulatory agency, recollection alone is not enough.
Take notes, always, warns Mr West.
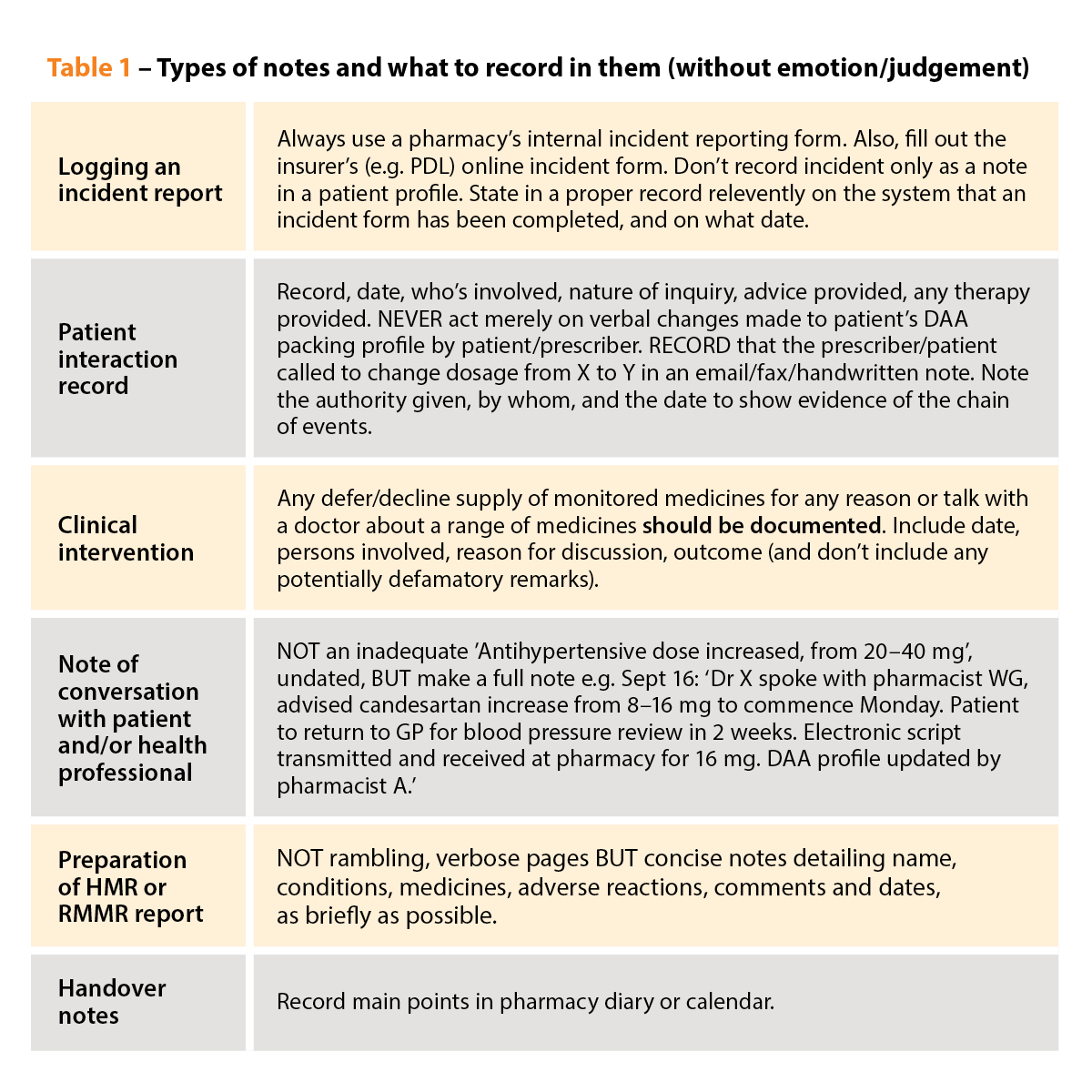
Top tips for note-taking
- If in doubt RECORD an interaction, especially when there is the potential for consequences – and the more thorough the better
- Abbreviations must be clear, consistent and able to be interpreted
- Emotive, judgemental or discriminatory language has no place in any notes
- If it isn’t documented, it didn’t happen!
Case study

Kate Gunthorpe MPS
Pharmacist Implementation & Change Specialist at TerryWhite Chemmart
Adjunct Lecturer –Scope of Practice at James Cook University,
Townsville & Brisbane, Queensland
As a Pharmacist Prescriber, educator and mentor for pharmacists studying and implementing change, I frequently emphasise the importance of clinical notetaking.
Clear, structured and accurate notes ensure continuity of care, facilitate professional communication, and meet medico-legal requirements. With expanding scope of practice services including smoking cessation and other patient-centred care, strong documentation skills are vital for every single pharmacist.
Well-documented patient interactions protect against medico-legal risks, whilst poor documentation may be seen as negligent or expose a pharmacist to unnecessary risk should an incident occur.
Here are my key dos and don’ts to help pharmacists elevate note-taking skills.
Dos
- Be objective: Facts are paramount. Instead of ‘the patient appears well’, document: ‘patient has good colour, sitting comfortably, speaking in full sentences alert to date, location and name’.
- Use a framework: SOAP format (Subjective, Objective, Assessment, Plan) helps organise notes and ensures nothing is missed.
- Record immediately: Documenting right after a consultation ensures notes are accurate and detailed.
- Be specific: Details such as ‘BP 145/85 mmHg on pre & post consultation readings’ are specific and objective, compared to ‘high blood pressure’.
- Report relevant findings: Negative findings are as important as positive findings. Documenting ‘patient denies chest tightness, radiating pain to the arm or jaw, shortness of breath’ is crucial, as is recording ‘patient reports intermittent chest pain lasting 5 minutes, triggered by exertion’.
Don’ts
- Be subjective: Avoid writing comments like ‘non-compliant patient’. Instead, document specifics: ‘patient missed medication doses due to misunderstanding instructions’.
- Delete notes: If an adjustment is needed, create a new entry electronically or strike through errors with a single line. Add the date and initial any changes.



 Pharmacists have always prescribed, but they have the potential to prescribe much more
Pharmacists have always prescribed, but they have the potential to prescribe much more



 Sponsorship information
Sponsorship information


 Talking to patients who have questions
Talking to patients who have questions







