td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28313
[post_author] => 3410
[post_date] => 2024-11-25 12:46:22
[post_date_gmt] => 2024-11-25 01:46:22
[post_content] => These oft-used medicines have become the analgesia of choice for many prescribers. But care should be taken before prescribing gabapentinoids to certain patients.
Gabapentinoid medicines are widely prescribed in Australia. Considered a safer alternative to opioids for neuropathic pain, there was an 8-fold increase in prescriptions for gabapentinoids from 2012 to 2018 – with 1 in 7 Australians aged 80 and older prescribed a gabapentinoid.
[caption id="attachment_28316" align="aligncenter" width="1280"]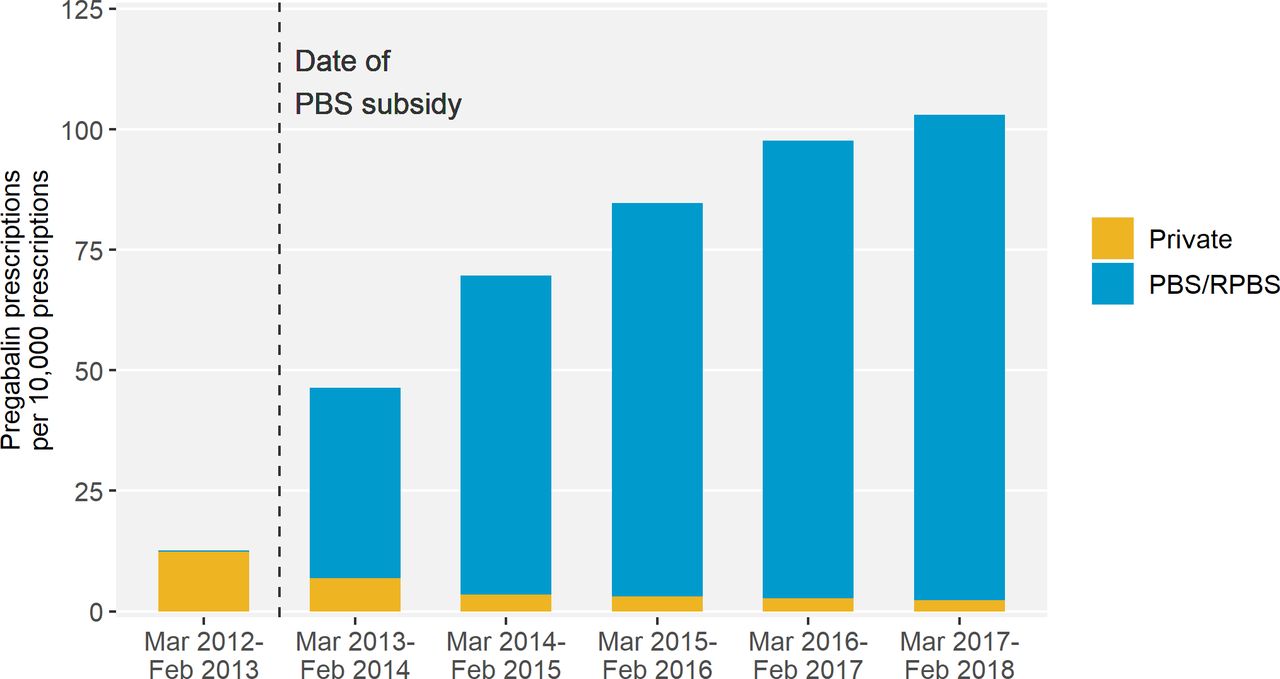 Source – Pregabalin prescribing patterns in Australian general practice, 2012–2018: a cross-sectional study[/caption]
But a new study from Monash University researchers, including pharmacists Miriam Leung and Professor Simon Bell FPS, found that harm can be caused within 2 months of initiation.
Over a 5-year period, the researchers analysed data for 28,293 patients in Victoria who experienced hip fractures.
‘Our research found that patients who were recently dispensed either pregabalin or gabapentin had 30% higher odds of experiencing a hip fracture,’ Prof Bell told Australian Pharmacist.
Source – Pregabalin prescribing patterns in Australian general practice, 2012–2018: a cross-sectional study[/caption]
But a new study from Monash University researchers, including pharmacists Miriam Leung and Professor Simon Bell FPS, found that harm can be caused within 2 months of initiation.
Over a 5-year period, the researchers analysed data for 28,293 patients in Victoria who experienced hip fractures.
‘Our research found that patients who were recently dispensed either pregabalin or gabapentin had 30% higher odds of experiencing a hip fracture,’ Prof Bell told Australian Pharmacist.
Who is most at risk?
The link between gabapentinoid use and hip fractures existed across different age groups.
However, the risk of hip fracture associated with gabapentinoid medicines was highest in patients who were frail or had renal impairment, said Prof Bell.
‘Frail older people are prone to falls and fractures,’ he said. ‘One in 25 adults aged 80 years and older experience a hip fracture each year.’
The impact of these incidents can be fatal.
‘Around one in four people who experience a hip fracture die within 12 months,’ said Prof Bell.
How should pharmacists assess and manage falls risk?
For certain neuropathic pain conditions such as postherpetic neuralgia, diabetic neuropathy, and mixed or post-traumatic neuropathy, gabapentinoids such as pregabalin or gabapentin can provide effective relief.
However, while approved by the Australian Therapeutic Goods Administration for refractory focal (partial) epilepsy and neuropathic pain, gabapentin and pregabalin are often prescribed off label – with limited evidence to support efficacy for off-label indications.
In patients who are likely to see some benefit of therapy, pharmacists should advise patients how to minimise risk before dispensing these medicines.
‘The risk of falls is highest at the start of treatment,’ said Prof Bell.
‘Therefore, it’s important that pharmacists and other clinicians advise on strategies to minimise falls risk at this time. This could include avoidance of other falls-risk increasing substances such as alcohol.’
Evaluating what other medicines at-risk patients are prescribed is also an important strategy for preventing harm.
‘It’s known that gabapentinoids can cause side-effects such as drowsiness, sedation and dizziness,’ said Prof Bell.
‘These side-effects may increase the risk of falls, particularly if gabapentinoids are co-administrated with other psychotropic or cardiovascular falls risk medications.’
What impact can dose have on falls risk?
Given risk is highest at the outset of treatment, the starting dose of gabapentinoids can also have an impact on the likelihood of falls.
‘It’s advisable that patients start with a low dose and titrate slowly,’ said Prof Bell. ‘This particularly applies to people who are frail or have renal impairment.’
When is a discussion with the prescriber warranted?
The ongoing need for gabapentinoid treatment for neuropathic pain should be reviewed regularly, said Prof Bell.
‘If patients do not experience benefit after an adequate trial of treatment, then gradual discontinuation may be warranted,’ he said.
However, it’s important to advise people who take a gabapentinoid medicine that they shouldn’t stop taking their medication without first speaking with their prescriber or pharmacist first.
‘Stopping gabapentinoid medications abruptly can cause withdrawal symptoms,’ Prof Bell added.
[post_title] => Neuropathic pain medicines can increase the risk of falls
[post_excerpt] =>
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => neuropathic-pain-medicines-can-increase-the-risk-of-falls
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-25 15:20:38
[post_modified_gmt] => 2024-11-25 04:20:38
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28313
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Neuropathic pain medicines can increase the risk of falls
[title] => Neuropathic pain medicines can increase the risk of falls
[href] => https://www.australianpharmacist.com.au/neuropathic-pain-medicines-can-increase-the-risk-of-falls/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28319
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28263
[post_author] => 3410
[post_date] => 2024-11-20 13:37:02
[post_date_gmt] => 2024-11-20 02:37:02
[post_content] => Australia’s understanding and adoption of Quality Use of Medicines (QUM) principles across general practice and primary care has led to overall improvements in medicine use, such as curtailing high-dose use of proton pump inhibitors.
But the challenge has since changed, with Australians living longer – resulting in an older, sicker population who uses more medicines, said Professor Libby Roughead – Director of the QUM and Pharmacy Research Centre at the University of South Australia.
‘Now the game is to say, how do we go forward when we’ve got a frail older population, and lots of specialty medicine? she asked.
This is the question a panel of experts sought to answer at the National Medicines Symposium 2024 yesterday (19 November).
Be wary of using ‘wonder drugs’ in older patients
When clinical trials are conducted on new medicines, they’re not tested in the over 65 age group, said Steve Waller, Senior Advisor, Medication without Harm, Australian Commission on Safety and Quality in Health Care.
[caption id="attachment_28267" align="alignnone" width="800"] National Medicines Symposium 2024 speakers (L to R): Steve Waller, Professor Jennifer Martin, Professor Libby Roughead, Tegan Taylor[/caption]
‘That creates complications, because we often don’t know what the impact in that older age group is … and pharmaceutical companies don’t have that information when they’re making an application for a new drug to be listed with the TGA [Therapeutic Goods Administration] and PBS [Pharmaceutical Benefits Scheme],’ he said.
Healthcare professionals must have awareness of the limitations of the data, thinks Professor Jennifer Martin, clinical pharmacologist and president of the Royal Australian College of Physicians.
‘Often, I say to people “why are you using a statin in [an older] population? We know the life expectancy when you go to a nursing home is less than 2 years, and you have to be on this drug at this dose for 5 years just to see a small reduction in a composite end point”,’ she said.
Healthcare professionals should rely on Australia’s ‘good sources of objective information’ such as Therapeutic Guidelines and the Australian Medicines Handbook, said Prof Roughead.
But more work needs to be done on increasing uptake of non-pharmacological interventions that are suitable for many conditions, including art therapy, music therapy, exercise and diet.
‘We know compassion practices are really helpful in some of the hard-to-treat conditions [such as] pain and depression, so we need to get better at involving the whole therapeutic armamentarium,’ she said. ‘The first definition of QUM is judicious selection of management options.’
National Medicines Symposium 2024 speakers (L to R): Steve Waller, Professor Jennifer Martin, Professor Libby Roughead, Tegan Taylor[/caption]
‘That creates complications, because we often don’t know what the impact in that older age group is … and pharmaceutical companies don’t have that information when they’re making an application for a new drug to be listed with the TGA [Therapeutic Goods Administration] and PBS [Pharmaceutical Benefits Scheme],’ he said.
Healthcare professionals must have awareness of the limitations of the data, thinks Professor Jennifer Martin, clinical pharmacologist and president of the Royal Australian College of Physicians.
‘Often, I say to people “why are you using a statin in [an older] population? We know the life expectancy when you go to a nursing home is less than 2 years, and you have to be on this drug at this dose for 5 years just to see a small reduction in a composite end point”,’ she said.
Healthcare professionals should rely on Australia’s ‘good sources of objective information’ such as Therapeutic Guidelines and the Australian Medicines Handbook, said Prof Roughead.
But more work needs to be done on increasing uptake of non-pharmacological interventions that are suitable for many conditions, including art therapy, music therapy, exercise and diet.
‘We know compassion practices are really helpful in some of the hard-to-treat conditions [such as] pain and depression, so we need to get better at involving the whole therapeutic armamentarium,’ she said. ‘The first definition of QUM is judicious selection of management options.’
Involve older patients in deprescribing decisions
Doctors, pharmacists, family members and carers typically talk among themselves about an older patient's medicine regimen. But it’s the patient they need to focus on, thinks Prof Martin.
‘When you talk to an older person, they will typically say “I don’t know why they started those pills” or “I don’t think I was supposed to be on them long-term, but no one stopped them, so I just kept taking them”,’ she said.
‘So, come back to the patient and ask, “Why are you taking these medications? What are your goals of care? Do you want pain relief? What are you looking for?”’
As patients reach their final chapter, many are just after quality of life – which doesn’t necessarily entail losing cognitive function through heavy use of opioids.
‘Opioids may play some role in pain, but they certainly take away a lot of the quality of life for older people,’ said Prof Martin. ‘It’s not until you spend time talking to the person that you find out they actually want to be very sharp; they think they can cope with their pain by other measures, and we can probably reduce some of their opioids.’
Warranted distrust in medicines and healthcare needs to be built back up
While we live in an age where misinformation is rife, some of it stems from the health system and pharma model, said Prof Martin.
‘For example, we know with gabapentin, which some people use for pain, most of the information that got onto the market was fraudulent,’ she said. ‘[There] was then a big investigation, with lawsuits still ongoing.’
The same goes for opioids, ineffective for many of the conditions they are prescribed for – particularly chronic pain.
‘The public are looking at their health providers saying, “We now know this is misinformation, but you prescribed this”, so we’ve lost a bit of engagement with our community,’ said Prof Martin.
With many patients with chronic pain on high doses of opioids that are not treating their conditions and impairing their quality of life, Prof Martin thinks the healthcare sector has ‘something to answer for’.
‘That misinformation is coming from industry and from the fact that we’re too busy to actually go back to their source material,’ she said.
The good news is that opioid deaths have decreased over the last 5 years in Australia, thanks to tighter prescribing regulations and better resources such as the Opioid Analgesic Stewardship in Acute Pain Clinical Care Standard, said Mr Waller.
Work on state formularies has also reduced the number of opioids that people can prescribe, said Prof Martin.
‘It has helped to get that conversation going of “Why do you need to have access to 10 different opioids in an in-patient setting?” and “Why do you need all these different concentrations?”’ she said.
However, more changes in practice are required to ensure that trend continues in the right direction, said Mr Waller.
‘We need to stop using opioids for chronic pain,’ he said. ‘There’s limited to no evidence to suggest that they work, and we need to be very judicious about our use of modified-release opioid analgesics.’
Yet as that work is done, it’s crucial to remember that these patients are suffering and compassion should be brought to the encounter – rather than simply saying ‘you can’t have that’, said Prof Roughead.
‘It’s not just ceasing a medicine. It’s ceasing a medicine and starting other things that you might need to help you be well, whether it be an exercise program or psychological services,’ she said.
Pharmacists can bridge communication and healthcare gaps in RACFs
With the Aged Care On-site Pharmacist (ACOP) program kicking off on 1 July 2024, pharmacists can improve the approach to healthcare by simply getting to know people – a skill well-honed by pharmacists in other settings, said Prof Roughead.
This includes understanding patient preferences and non-pharmacological activities that might support them.
‘If we can build a system where we can create relationships, particularly in a virtual world … we’re all going to be safer and we’re all going to feel better,’ she said.
‘That’s got to be the strength of an embedded pharmacist in aged care, that day-to-day knowledge of what the patient’s likes and dislikes are and how they’ve been managed over a continuum, as opposed to a visit that might happen once a year,’ added Mr Waller.
As the custodian of the pharmacy profession’s Professional Practice Standards and an education and training provider, PSA has continued to invest and embark into practice support training and education for pharmacists to become ACOP credentialed, said PSA National President Associated Professor Fei Sim.
The training covers all elements of this role – from professionalism, to understanding the governance of an RACF, collaborative practice, providing person-centred medication management and working within a multidisciplinary team to improve the safe and quality use of medicines.
‘Pharmacists undertaking the training program would then acquire the necessary credentials, qualifications and skill set to be able to undertake the role as an aged care on-site pharmacist,’ she said.
‘We’re also providing ongoing resources and clinical updates for credentialed pharmacists so they can be kept up to date with their knowledge and skills to undertake the role.’
With any new areas of practice, there is a great need for mentoring and networking for like-minded pharmacists who work in the same area to forge bonds, said A/Prof Sim. ‘That’s why PSA created the Consultant Pharmacists CSI group [and] an annual Consultant Pharmacist Conference, focusing on supporting and meeting the learning needs of credentialed pharmacists.’
[post_title] => Giving a voice back to elderly patients
[post_excerpt] => Yesterday’s National Medicine Symposium delivered a stark critique of how our health system is failing older patients – and how to fix it.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => giving-a-voice-back-to-elderly-patients
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-20 15:44:59
[post_modified_gmt] => 2024-11-20 04:44:59
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28263
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Giving a voice back to elderly patients
[title] => Giving a voice back to elderly patients
[href] => https://www.australianpharmacist.com.au/giving-a-voice-back-to-elderly-patients/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28266
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28254
[post_author] => 3410
[post_date] => 2024-11-18 13:05:58
[post_date_gmt] => 2024-11-18 02:05:58
[post_content] => Mpox cases are surging in Australia. An expert reveals how pharmacists can address the rising spread.
When mpox was first reported in Australia in May 2022, case numbers remained relatively low for the better part of 2 years.
However, in 2024 there has been a significant spike in case numbers in several Australian states and territories, with New South Wales, Victoria and Western Australia all seeing rising locally acquired notifications.
In September, it was reported that mpox cases grew a staggering 570% since July 2024 –with over 724 cases recorded this year. Yet vaccination rates remain low.
Meanwhile, cases of clade Ib – which has a much higher fatality rate than clade IIb strain spreading in Australia – have been detected in numerous countries around the world, most recently the United States. The worldwide spread of the new clade led the World Health Organisation to declare the mpox outbreak a public health emergency of international concern.
At this stage, pharmacists can only administer the mpox vaccine in Victoria and the Northern Territory.
However, pharmacists in all jurisdictions have an essential role in raising awareness of vaccine eligibility and dosing schedule, when to get vaccinated and where to get tested – all of which can help to bring down rising case numbers.
Watch the video below to hear sexual health expert Dr Tom Morley explain how pharmacists can go about this in a culturally safe way.
https://www.youtube.com/watch?v=ZPzbadkq8sM
[post_title] => Curbing the spread as mpox cases skyrocket
[post_excerpt] => Mpox cases are surging both in Australia and around the world. An expert reveals how pharmacists can address the rising spread.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => curbing-the-spread-as-mpox-cases-skyrocket
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-18 15:16:33
[post_modified_gmt] => 2024-11-18 04:16:33
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28254
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Curbing the spread as mpox cases skyrocket
[title] => Curbing the spread as mpox cases skyrocket
[href] => https://www.australianpharmacist.com.au/curbing-the-spread-as-mpox-cases-skyrocket/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28257
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28190
[post_author] => 46
[post_date] => 2024-11-18 09:28:17
[post_date_gmt] => 2024-11-17 22:28:17
[post_content] => Constipation can be an embarrassing topic to discuss with your patients. But irregular bowel movements can not only be uncomfortable, but can lead to other health conditions and severely impact a patient’s quality of life.
[caption id="attachment_28205" align="alignright" width="150"] This CPD activity is sponsored by Reckitt. All content is the true, accurate and independent opinion of the speakers and the views expressed are entirely their own.[/caption]
Constipation is a common problem in the community,1 that can significantly impact quality of life if not properly managed.2 It’s also a common reason for primary care visits and referrals to gastroenterologists.3 Unfortunately, many patients are choosing laxatives without the help and advice of a health professional1 so may be choosing products that don’t work effectively5 or choosing to use laxatives when addressing dietary, lifestyle or medicine regimens may be the most appropriate course of action. In this CPD accredited podcast, listen to Priceline Health Services Manager Brett Macfarlane and Senior Clinical Pharmacist – Gastroenterology at the Royal Melbourne Hospital Stephanie Dimovski discuss the problem of constipation and how pharmacists can assist patients in managing this condition. They will address the importance of identifying whether insufficient fibre and fluid intake may be contributing and whether making dietary and exercise recommendations is enough to restore normal bowel habits.
This CPD activity is sponsored by Reckitt. All content is the true, accurate and independent opinion of the speakers and the views expressed are entirely their own.[/caption]
Constipation is a common problem in the community,1 that can significantly impact quality of life if not properly managed.2 It’s also a common reason for primary care visits and referrals to gastroenterologists.3 Unfortunately, many patients are choosing laxatives without the help and advice of a health professional1 so may be choosing products that don’t work effectively5 or choosing to use laxatives when addressing dietary, lifestyle or medicine regimens may be the most appropriate course of action. In this CPD accredited podcast, listen to Priceline Health Services Manager Brett Macfarlane and Senior Clinical Pharmacist – Gastroenterology at the Royal Melbourne Hospital Stephanie Dimovski discuss the problem of constipation and how pharmacists can assist patients in managing this condition. They will address the importance of identifying whether insufficient fibre and fluid intake may be contributing and whether making dietary and exercise recommendations is enough to restore normal bowel habits.
After reading this article, pharmacists should be able to:
|
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28164
[post_author] => 3410
[post_date] => 2024-11-13 12:50:58
[post_date_gmt] => 2024-11-13 01:50:58
[post_content] => The Therapeutic Goods Administration (TGA) has worked with Phenergan manufacturer Sanofi to develop a new contraindication for the medicine in children under 6.
The decision to restrict use of the medicine in this age cohort – commonly used to treat allergies, travel sickness and nausea – is based on a thorough evaluation of new scientific evidence that the risks outweigh the benefits, a spokesperson for Sanofi told Australian Pharmacist.
‘Following recent evaluations made by Sanofi Consumer Healthcare Pty Ltd, including a benefit-risk assessment, the research has shown a causal association between promethazine and safety concerns,’ said this spokesperson.
The sponsor-initiated update was prompted by advice from the TGA Advisory Committee on Medicines (ACM) – first-generation oral sedating antihistamines – do not use in children, said a spokesperson from the TGA.
‘Further review by the sponsor of cumulative safety data in children 2 to 5 years of age demonstrated sufficient evidence of a causal association between promethazine and psychiatric and central nervous system adverse events in this age group,’ the TGA spokesperson told AP.
The contraindication comes after Medsafe, the New Zealand Medicines and Medical Devices Safety Authority, moved to contraindicate the use of the medicine in children under 6 due to the potential for fatal respiratory depression, psychiatric and central nervous system (CNS) events.
AP understands that the contraindication will affect other products. A spokesperson for AFT said a variation has been submitted to update the product information and label on Allersoothe Elixir with a change to the age indication from children 2 years and older to children 6 years and older. This submission is pending approval.
Will the packaging change?
Not immediately.
New labels for promethazine-containing products will be rolled out in 2025 due to production and logistics lead times, said the Sanofi spokesperson.
‘No immediate action is required regarding current stock. There is no need to set aside existing medications, as this communication does not constitute a recall,’ said the spokesperson. ‘Similarly, the revised labels do not create any changes in the ordering process.
The product information for Phenergan has been updated and is available here.
What should pharmacists do if they get a Phenergan script for an 18 month old infant?
The use of promethazine in children under 6 years of age is now both contraindicated and off label, said Peter Guthrey MPS, PSA Senior Pharmacist – strategic policy.
‘This means that if you choose to dispense, both the prescriber and dispenser carry the full indemnity risk, and you need to get the patient to provide informed consent,’ he said.
Should a parent present with a script for promethazine for use in a child under 6 years of age, pharmacists should contact the prescriber to discuss the risks and benefits, noting that it's contraindicated.
Is there any situation where it would be appropriate to dispense Phenergan to a young child?
It would need to be a pretty compelling case, where the benefit to a child outweighed the risk of respiratory depression, psychiatric or CNS events, said Mr Guthrey.
‘Given it’s a documented contraindication, it'd be pretty hard to demonstrate the medicine is ‘‘safe and therapeutically appropriate’’,’ he said.
‘It is going to be difficult to find a situation where supply is clinically justified and pharmacists have met their obligations to patient safety.’
What about prescribing Phenergan as a Schedule 3 medicine?
If a parent requests promethazine as a Schedule 3 medicine for someone under the age of 6 years, generally alternate products or advice for treatment should be provided following a discussion.
‘While a pharmacist prescribing promethazine as a Pharmacist Only Medicine is lawful for children aged 2-5 years, it is still contraindicated,’ said Mr Guthrey. ‘There would be very few, if any, situations where prescribing the medicine where contraindicated would be warranted.’
What about phenylephrine?
There are some combination phenylephrine products indicated for children under 6 years of age for nasal congestion. However, there is plenty of evidence showing that oral phenylephrine products are ineffective as a nasal decongestant.
In fact, the United States Food and Drug Administration (FDA) recently announced it will move to ban oral phenylephrine products because they simply don't work.
‘Based on our review of available data, and consistent with the advice of the advisory committee, we are taking this next step in the process to propose removing oral phenylephrine because it is not effective as a nasal decongestant,’ said Patrizia Cavazzoni, M.D., director of the FDA’s Center for Drug Evaluation and Research.
While a spokesperson for the TGA told Australian Pharmacist back in July that there are ‘no plans’ to review the effectiveness of oral phenylephrine, it will continue to monitor the outcomes of the FDA review.
What advice should pharmacists provide?
For children with allergies, non-sedating antihistamines are first line.
The best thing parents can do when a child under 6 years of age has cough or cold symptoms is to wait it out, with a review by a medical practitioner when appropriate.
‘It's about reassurance to parents that the cough in itself isn't harmful, and that kids don’t always need medicines for a cold – they need time and supportive therapy,’ said Mr Guthrey.
It’s important that pharmacists give parents confidence that they're doing the right thing by not treating the cough, and providing symptomatic relief for fever and chills – ensuring they are appropriately counselled on when review by a medical practitioner may be appropriate.
For more information, refer to the Australian Pharmaceutical Formulary and Handbook treatment guidelines on:
[post_title] => Do not supply Phenergan to children under 6, manufacturer warns
[post_excerpt] => The TGA has worked with Phenergan manufacturer Sanofi to develop a new contraindication for the medicine in children under 6.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => do-not-supply-phenergan-to-children-under-6-manufacturer-warns
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-21 09:54:51
[post_modified_gmt] => 2024-11-20 22:54:51
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28164
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Do not supply Phenergan to children under 6, manufacturer warns
[title] => Do not supply Phenergan to children under 6, manufacturer warns
[href] => https://www.australianpharmacist.com.au/do-not-supply-phenergan-to-children-under-6-manufacturer-warns/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28167
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28313
[post_author] => 3410
[post_date] => 2024-11-25 12:46:22
[post_date_gmt] => 2024-11-25 01:46:22
[post_content] => These oft-used medicines have become the analgesia of choice for many prescribers. But care should be taken before prescribing gabapentinoids to certain patients.
Gabapentinoid medicines are widely prescribed in Australia. Considered a safer alternative to opioids for neuropathic pain, there was an 8-fold increase in prescriptions for gabapentinoids from 2012 to 2018 – with 1 in 7 Australians aged 80 and older prescribed a gabapentinoid.
[caption id="attachment_28316" align="aligncenter" width="1280"]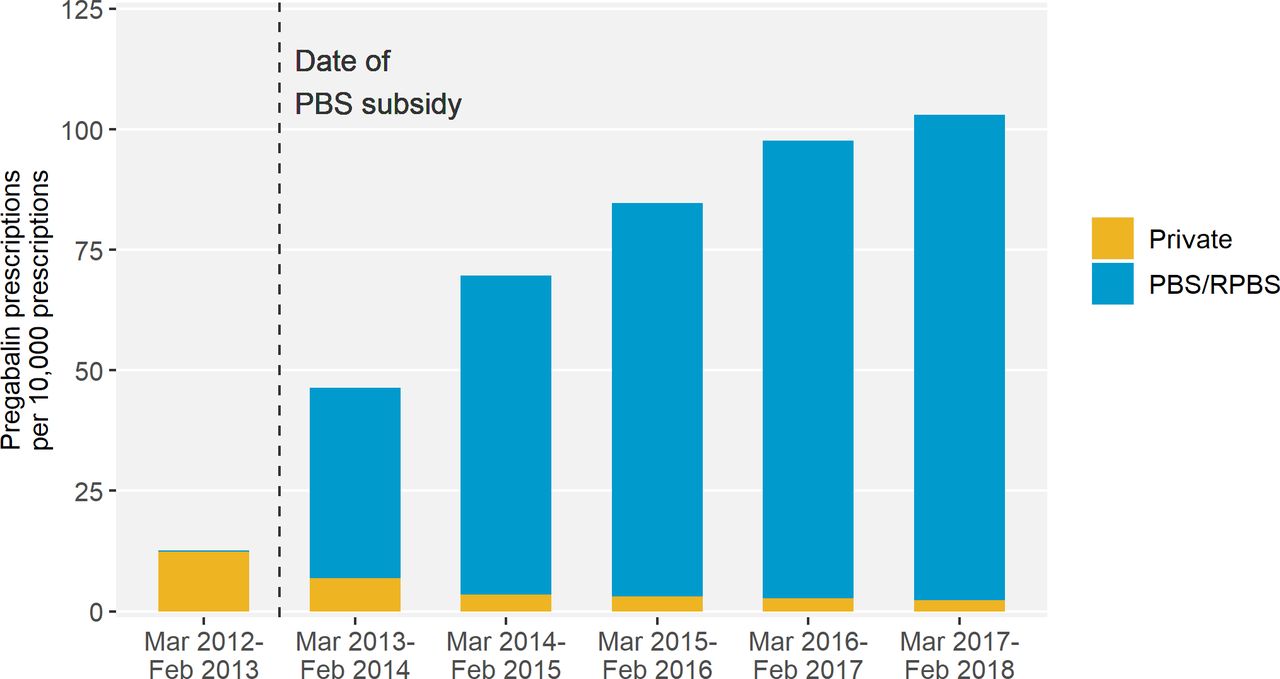 Source – Pregabalin prescribing patterns in Australian general practice, 2012–2018: a cross-sectional study[/caption]
But a new study from Monash University researchers, including pharmacists Miriam Leung and Professor Simon Bell FPS, found that harm can be caused within 2 months of initiation.
Over a 5-year period, the researchers analysed data for 28,293 patients in Victoria who experienced hip fractures.
‘Our research found that patients who were recently dispensed either pregabalin or gabapentin had 30% higher odds of experiencing a hip fracture,’ Prof Bell told Australian Pharmacist.
Source – Pregabalin prescribing patterns in Australian general practice, 2012–2018: a cross-sectional study[/caption]
But a new study from Monash University researchers, including pharmacists Miriam Leung and Professor Simon Bell FPS, found that harm can be caused within 2 months of initiation.
Over a 5-year period, the researchers analysed data for 28,293 patients in Victoria who experienced hip fractures.
‘Our research found that patients who were recently dispensed either pregabalin or gabapentin had 30% higher odds of experiencing a hip fracture,’ Prof Bell told Australian Pharmacist.
Who is most at risk?
The link between gabapentinoid use and hip fractures existed across different age groups.
However, the risk of hip fracture associated with gabapentinoid medicines was highest in patients who were frail or had renal impairment, said Prof Bell.
‘Frail older people are prone to falls and fractures,’ he said. ‘One in 25 adults aged 80 years and older experience a hip fracture each year.’
The impact of these incidents can be fatal.
‘Around one in four people who experience a hip fracture die within 12 months,’ said Prof Bell.
How should pharmacists assess and manage falls risk?
For certain neuropathic pain conditions such as postherpetic neuralgia, diabetic neuropathy, and mixed or post-traumatic neuropathy, gabapentinoids such as pregabalin or gabapentin can provide effective relief.
However, while approved by the Australian Therapeutic Goods Administration for refractory focal (partial) epilepsy and neuropathic pain, gabapentin and pregabalin are often prescribed off label – with limited evidence to support efficacy for off-label indications.
In patients who are likely to see some benefit of therapy, pharmacists should advise patients how to minimise risk before dispensing these medicines.
‘The risk of falls is highest at the start of treatment,’ said Prof Bell.
‘Therefore, it’s important that pharmacists and other clinicians advise on strategies to minimise falls risk at this time. This could include avoidance of other falls-risk increasing substances such as alcohol.’
Evaluating what other medicines at-risk patients are prescribed is also an important strategy for preventing harm.
‘It’s known that gabapentinoids can cause side-effects such as drowsiness, sedation and dizziness,’ said Prof Bell.
‘These side-effects may increase the risk of falls, particularly if gabapentinoids are co-administrated with other psychotropic or cardiovascular falls risk medications.’
What impact can dose have on falls risk?
Given risk is highest at the outset of treatment, the starting dose of gabapentinoids can also have an impact on the likelihood of falls.
‘It’s advisable that patients start with a low dose and titrate slowly,’ said Prof Bell. ‘This particularly applies to people who are frail or have renal impairment.’
When is a discussion with the prescriber warranted?
The ongoing need for gabapentinoid treatment for neuropathic pain should be reviewed regularly, said Prof Bell.
‘If patients do not experience benefit after an adequate trial of treatment, then gradual discontinuation may be warranted,’ he said.
However, it’s important to advise people who take a gabapentinoid medicine that they shouldn’t stop taking their medication without first speaking with their prescriber or pharmacist first.
‘Stopping gabapentinoid medications abruptly can cause withdrawal symptoms,’ Prof Bell added.
[post_title] => Neuropathic pain medicines can increase the risk of falls
[post_excerpt] =>
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => neuropathic-pain-medicines-can-increase-the-risk-of-falls
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-25 15:20:38
[post_modified_gmt] => 2024-11-25 04:20:38
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28313
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Neuropathic pain medicines can increase the risk of falls
[title] => Neuropathic pain medicines can increase the risk of falls
[href] => https://www.australianpharmacist.com.au/neuropathic-pain-medicines-can-increase-the-risk-of-falls/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28319
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28263
[post_author] => 3410
[post_date] => 2024-11-20 13:37:02
[post_date_gmt] => 2024-11-20 02:37:02
[post_content] => Australia’s understanding and adoption of Quality Use of Medicines (QUM) principles across general practice and primary care has led to overall improvements in medicine use, such as curtailing high-dose use of proton pump inhibitors.
But the challenge has since changed, with Australians living longer – resulting in an older, sicker population who uses more medicines, said Professor Libby Roughead – Director of the QUM and Pharmacy Research Centre at the University of South Australia.
‘Now the game is to say, how do we go forward when we’ve got a frail older population, and lots of specialty medicine? she asked.
This is the question a panel of experts sought to answer at the National Medicines Symposium 2024 yesterday (19 November).
Be wary of using ‘wonder drugs’ in older patients
When clinical trials are conducted on new medicines, they’re not tested in the over 65 age group, said Steve Waller, Senior Advisor, Medication without Harm, Australian Commission on Safety and Quality in Health Care.
[caption id="attachment_28267" align="alignnone" width="800"] National Medicines Symposium 2024 speakers (L to R): Steve Waller, Professor Jennifer Martin, Professor Libby Roughead, Tegan Taylor[/caption]
‘That creates complications, because we often don’t know what the impact in that older age group is … and pharmaceutical companies don’t have that information when they’re making an application for a new drug to be listed with the TGA [Therapeutic Goods Administration] and PBS [Pharmaceutical Benefits Scheme],’ he said.
Healthcare professionals must have awareness of the limitations of the data, thinks Professor Jennifer Martin, clinical pharmacologist and president of the Royal Australian College of Physicians.
‘Often, I say to people “why are you using a statin in [an older] population? We know the life expectancy when you go to a nursing home is less than 2 years, and you have to be on this drug at this dose for 5 years just to see a small reduction in a composite end point”,’ she said.
Healthcare professionals should rely on Australia’s ‘good sources of objective information’ such as Therapeutic Guidelines and the Australian Medicines Handbook, said Prof Roughead.
But more work needs to be done on increasing uptake of non-pharmacological interventions that are suitable for many conditions, including art therapy, music therapy, exercise and diet.
‘We know compassion practices are really helpful in some of the hard-to-treat conditions [such as] pain and depression, so we need to get better at involving the whole therapeutic armamentarium,’ she said. ‘The first definition of QUM is judicious selection of management options.’
National Medicines Symposium 2024 speakers (L to R): Steve Waller, Professor Jennifer Martin, Professor Libby Roughead, Tegan Taylor[/caption]
‘That creates complications, because we often don’t know what the impact in that older age group is … and pharmaceutical companies don’t have that information when they’re making an application for a new drug to be listed with the TGA [Therapeutic Goods Administration] and PBS [Pharmaceutical Benefits Scheme],’ he said.
Healthcare professionals must have awareness of the limitations of the data, thinks Professor Jennifer Martin, clinical pharmacologist and president of the Royal Australian College of Physicians.
‘Often, I say to people “why are you using a statin in [an older] population? We know the life expectancy when you go to a nursing home is less than 2 years, and you have to be on this drug at this dose for 5 years just to see a small reduction in a composite end point”,’ she said.
Healthcare professionals should rely on Australia’s ‘good sources of objective information’ such as Therapeutic Guidelines and the Australian Medicines Handbook, said Prof Roughead.
But more work needs to be done on increasing uptake of non-pharmacological interventions that are suitable for many conditions, including art therapy, music therapy, exercise and diet.
‘We know compassion practices are really helpful in some of the hard-to-treat conditions [such as] pain and depression, so we need to get better at involving the whole therapeutic armamentarium,’ she said. ‘The first definition of QUM is judicious selection of management options.’
Involve older patients in deprescribing decisions
Doctors, pharmacists, family members and carers typically talk among themselves about an older patient's medicine regimen. But it’s the patient they need to focus on, thinks Prof Martin.
‘When you talk to an older person, they will typically say “I don’t know why they started those pills” or “I don’t think I was supposed to be on them long-term, but no one stopped them, so I just kept taking them”,’ she said.
‘So, come back to the patient and ask, “Why are you taking these medications? What are your goals of care? Do you want pain relief? What are you looking for?”’
As patients reach their final chapter, many are just after quality of life – which doesn’t necessarily entail losing cognitive function through heavy use of opioids.
‘Opioids may play some role in pain, but they certainly take away a lot of the quality of life for older people,’ said Prof Martin. ‘It’s not until you spend time talking to the person that you find out they actually want to be very sharp; they think they can cope with their pain by other measures, and we can probably reduce some of their opioids.’
Warranted distrust in medicines and healthcare needs to be built back up
While we live in an age where misinformation is rife, some of it stems from the health system and pharma model, said Prof Martin.
‘For example, we know with gabapentin, which some people use for pain, most of the information that got onto the market was fraudulent,’ she said. ‘[There] was then a big investigation, with lawsuits still ongoing.’
The same goes for opioids, ineffective for many of the conditions they are prescribed for – particularly chronic pain.
‘The public are looking at their health providers saying, “We now know this is misinformation, but you prescribed this”, so we’ve lost a bit of engagement with our community,’ said Prof Martin.
With many patients with chronic pain on high doses of opioids that are not treating their conditions and impairing their quality of life, Prof Martin thinks the healthcare sector has ‘something to answer for’.
‘That misinformation is coming from industry and from the fact that we’re too busy to actually go back to their source material,’ she said.
The good news is that opioid deaths have decreased over the last 5 years in Australia, thanks to tighter prescribing regulations and better resources such as the Opioid Analgesic Stewardship in Acute Pain Clinical Care Standard, said Mr Waller.
Work on state formularies has also reduced the number of opioids that people can prescribe, said Prof Martin.
‘It has helped to get that conversation going of “Why do you need to have access to 10 different opioids in an in-patient setting?” and “Why do you need all these different concentrations?”’ she said.
However, more changes in practice are required to ensure that trend continues in the right direction, said Mr Waller.
‘We need to stop using opioids for chronic pain,’ he said. ‘There’s limited to no evidence to suggest that they work, and we need to be very judicious about our use of modified-release opioid analgesics.’
Yet as that work is done, it’s crucial to remember that these patients are suffering and compassion should be brought to the encounter – rather than simply saying ‘you can’t have that’, said Prof Roughead.
‘It’s not just ceasing a medicine. It’s ceasing a medicine and starting other things that you might need to help you be well, whether it be an exercise program or psychological services,’ she said.
Pharmacists can bridge communication and healthcare gaps in RACFs
With the Aged Care On-site Pharmacist (ACOP) program kicking off on 1 July 2024, pharmacists can improve the approach to healthcare by simply getting to know people – a skill well-honed by pharmacists in other settings, said Prof Roughead.
This includes understanding patient preferences and non-pharmacological activities that might support them.
‘If we can build a system where we can create relationships, particularly in a virtual world … we’re all going to be safer and we’re all going to feel better,’ she said.
‘That’s got to be the strength of an embedded pharmacist in aged care, that day-to-day knowledge of what the patient’s likes and dislikes are and how they’ve been managed over a continuum, as opposed to a visit that might happen once a year,’ added Mr Waller.
As the custodian of the pharmacy profession’s Professional Practice Standards and an education and training provider, PSA has continued to invest and embark into practice support training and education for pharmacists to become ACOP credentialed, said PSA National President Associated Professor Fei Sim.
The training covers all elements of this role – from professionalism, to understanding the governance of an RACF, collaborative practice, providing person-centred medication management and working within a multidisciplinary team to improve the safe and quality use of medicines.
‘Pharmacists undertaking the training program would then acquire the necessary credentials, qualifications and skill set to be able to undertake the role as an aged care on-site pharmacist,’ she said.
‘We’re also providing ongoing resources and clinical updates for credentialed pharmacists so they can be kept up to date with their knowledge and skills to undertake the role.’
With any new areas of practice, there is a great need for mentoring and networking for like-minded pharmacists who work in the same area to forge bonds, said A/Prof Sim. ‘That’s why PSA created the Consultant Pharmacists CSI group [and] an annual Consultant Pharmacist Conference, focusing on supporting and meeting the learning needs of credentialed pharmacists.’
[post_title] => Giving a voice back to elderly patients
[post_excerpt] => Yesterday’s National Medicine Symposium delivered a stark critique of how our health system is failing older patients – and how to fix it.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => giving-a-voice-back-to-elderly-patients
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-20 15:44:59
[post_modified_gmt] => 2024-11-20 04:44:59
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28263
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Giving a voice back to elderly patients
[title] => Giving a voice back to elderly patients
[href] => https://www.australianpharmacist.com.au/giving-a-voice-back-to-elderly-patients/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28266
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28254
[post_author] => 3410
[post_date] => 2024-11-18 13:05:58
[post_date_gmt] => 2024-11-18 02:05:58
[post_content] => Mpox cases are surging in Australia. An expert reveals how pharmacists can address the rising spread.
When mpox was first reported in Australia in May 2022, case numbers remained relatively low for the better part of 2 years.
However, in 2024 there has been a significant spike in case numbers in several Australian states and territories, with New South Wales, Victoria and Western Australia all seeing rising locally acquired notifications.
In September, it was reported that mpox cases grew a staggering 570% since July 2024 –with over 724 cases recorded this year. Yet vaccination rates remain low.
Meanwhile, cases of clade Ib – which has a much higher fatality rate than clade IIb strain spreading in Australia – have been detected in numerous countries around the world, most recently the United States. The worldwide spread of the new clade led the World Health Organisation to declare the mpox outbreak a public health emergency of international concern.
At this stage, pharmacists can only administer the mpox vaccine in Victoria and the Northern Territory.
However, pharmacists in all jurisdictions have an essential role in raising awareness of vaccine eligibility and dosing schedule, when to get vaccinated and where to get tested – all of which can help to bring down rising case numbers.
Watch the video below to hear sexual health expert Dr Tom Morley explain how pharmacists can go about this in a culturally safe way.
https://www.youtube.com/watch?v=ZPzbadkq8sM
[post_title] => Curbing the spread as mpox cases skyrocket
[post_excerpt] => Mpox cases are surging both in Australia and around the world. An expert reveals how pharmacists can address the rising spread.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => curbing-the-spread-as-mpox-cases-skyrocket
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-18 15:16:33
[post_modified_gmt] => 2024-11-18 04:16:33
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28254
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Curbing the spread as mpox cases skyrocket
[title] => Curbing the spread as mpox cases skyrocket
[href] => https://www.australianpharmacist.com.au/curbing-the-spread-as-mpox-cases-skyrocket/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28257
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28190
[post_author] => 46
[post_date] => 2024-11-18 09:28:17
[post_date_gmt] => 2024-11-17 22:28:17
[post_content] => Constipation can be an embarrassing topic to discuss with your patients. But irregular bowel movements can not only be uncomfortable, but can lead to other health conditions and severely impact a patient’s quality of life.
[caption id="attachment_28205" align="alignright" width="150"] This CPD activity is sponsored by Reckitt. All content is the true, accurate and independent opinion of the speakers and the views expressed are entirely their own.[/caption]
Constipation is a common problem in the community,1 that can significantly impact quality of life if not properly managed.2 It’s also a common reason for primary care visits and referrals to gastroenterologists.3 Unfortunately, many patients are choosing laxatives without the help and advice of a health professional1 so may be choosing products that don’t work effectively5 or choosing to use laxatives when addressing dietary, lifestyle or medicine regimens may be the most appropriate course of action. In this CPD accredited podcast, listen to Priceline Health Services Manager Brett Macfarlane and Senior Clinical Pharmacist – Gastroenterology at the Royal Melbourne Hospital Stephanie Dimovski discuss the problem of constipation and how pharmacists can assist patients in managing this condition. They will address the importance of identifying whether insufficient fibre and fluid intake may be contributing and whether making dietary and exercise recommendations is enough to restore normal bowel habits.
This CPD activity is sponsored by Reckitt. All content is the true, accurate and independent opinion of the speakers and the views expressed are entirely their own.[/caption]
Constipation is a common problem in the community,1 that can significantly impact quality of life if not properly managed.2 It’s also a common reason for primary care visits and referrals to gastroenterologists.3 Unfortunately, many patients are choosing laxatives without the help and advice of a health professional1 so may be choosing products that don’t work effectively5 or choosing to use laxatives when addressing dietary, lifestyle or medicine regimens may be the most appropriate course of action. In this CPD accredited podcast, listen to Priceline Health Services Manager Brett Macfarlane and Senior Clinical Pharmacist – Gastroenterology at the Royal Melbourne Hospital Stephanie Dimovski discuss the problem of constipation and how pharmacists can assist patients in managing this condition. They will address the importance of identifying whether insufficient fibre and fluid intake may be contributing and whether making dietary and exercise recommendations is enough to restore normal bowel habits.
After reading this article, pharmacists should be able to:
|
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28164
[post_author] => 3410
[post_date] => 2024-11-13 12:50:58
[post_date_gmt] => 2024-11-13 01:50:58
[post_content] => The Therapeutic Goods Administration (TGA) has worked with Phenergan manufacturer Sanofi to develop a new contraindication for the medicine in children under 6.
The decision to restrict use of the medicine in this age cohort – commonly used to treat allergies, travel sickness and nausea – is based on a thorough evaluation of new scientific evidence that the risks outweigh the benefits, a spokesperson for Sanofi told Australian Pharmacist.
‘Following recent evaluations made by Sanofi Consumer Healthcare Pty Ltd, including a benefit-risk assessment, the research has shown a causal association between promethazine and safety concerns,’ said this spokesperson.
The sponsor-initiated update was prompted by advice from the TGA Advisory Committee on Medicines (ACM) – first-generation oral sedating antihistamines – do not use in children, said a spokesperson from the TGA.
‘Further review by the sponsor of cumulative safety data in children 2 to 5 years of age demonstrated sufficient evidence of a causal association between promethazine and psychiatric and central nervous system adverse events in this age group,’ the TGA spokesperson told AP.
The contraindication comes after Medsafe, the New Zealand Medicines and Medical Devices Safety Authority, moved to contraindicate the use of the medicine in children under 6 due to the potential for fatal respiratory depression, psychiatric and central nervous system (CNS) events.
AP understands that the contraindication will affect other products. A spokesperson for AFT said a variation has been submitted to update the product information and label on Allersoothe Elixir with a change to the age indication from children 2 years and older to children 6 years and older. This submission is pending approval.
Will the packaging change?
Not immediately.
New labels for promethazine-containing products will be rolled out in 2025 due to production and logistics lead times, said the Sanofi spokesperson.
‘No immediate action is required regarding current stock. There is no need to set aside existing medications, as this communication does not constitute a recall,’ said the spokesperson. ‘Similarly, the revised labels do not create any changes in the ordering process.
The product information for Phenergan has been updated and is available here.
What should pharmacists do if they get a Phenergan script for an 18 month old infant?
The use of promethazine in children under 6 years of age is now both contraindicated and off label, said Peter Guthrey MPS, PSA Senior Pharmacist – strategic policy.
‘This means that if you choose to dispense, both the prescriber and dispenser carry the full indemnity risk, and you need to get the patient to provide informed consent,’ he said.
Should a parent present with a script for promethazine for use in a child under 6 years of age, pharmacists should contact the prescriber to discuss the risks and benefits, noting that it's contraindicated.
Is there any situation where it would be appropriate to dispense Phenergan to a young child?
It would need to be a pretty compelling case, where the benefit to a child outweighed the risk of respiratory depression, psychiatric or CNS events, said Mr Guthrey.
‘Given it’s a documented contraindication, it'd be pretty hard to demonstrate the medicine is ‘‘safe and therapeutically appropriate’’,’ he said.
‘It is going to be difficult to find a situation where supply is clinically justified and pharmacists have met their obligations to patient safety.’
What about prescribing Phenergan as a Schedule 3 medicine?
If a parent requests promethazine as a Schedule 3 medicine for someone under the age of 6 years, generally alternate products or advice for treatment should be provided following a discussion.
‘While a pharmacist prescribing promethazine as a Pharmacist Only Medicine is lawful for children aged 2-5 years, it is still contraindicated,’ said Mr Guthrey. ‘There would be very few, if any, situations where prescribing the medicine where contraindicated would be warranted.’
What about phenylephrine?
There are some combination phenylephrine products indicated for children under 6 years of age for nasal congestion. However, there is plenty of evidence showing that oral phenylephrine products are ineffective as a nasal decongestant.
In fact, the United States Food and Drug Administration (FDA) recently announced it will move to ban oral phenylephrine products because they simply don't work.
‘Based on our review of available data, and consistent with the advice of the advisory committee, we are taking this next step in the process to propose removing oral phenylephrine because it is not effective as a nasal decongestant,’ said Patrizia Cavazzoni, M.D., director of the FDA’s Center for Drug Evaluation and Research.
While a spokesperson for the TGA told Australian Pharmacist back in July that there are ‘no plans’ to review the effectiveness of oral phenylephrine, it will continue to monitor the outcomes of the FDA review.
What advice should pharmacists provide?
For children with allergies, non-sedating antihistamines are first line.
The best thing parents can do when a child under 6 years of age has cough or cold symptoms is to wait it out, with a review by a medical practitioner when appropriate.
‘It's about reassurance to parents that the cough in itself isn't harmful, and that kids don’t always need medicines for a cold – they need time and supportive therapy,’ said Mr Guthrey.
It’s important that pharmacists give parents confidence that they're doing the right thing by not treating the cough, and providing symptomatic relief for fever and chills – ensuring they are appropriately counselled on when review by a medical practitioner may be appropriate.
For more information, refer to the Australian Pharmaceutical Formulary and Handbook treatment guidelines on:
[post_title] => Do not supply Phenergan to children under 6, manufacturer warns
[post_excerpt] => The TGA has worked with Phenergan manufacturer Sanofi to develop a new contraindication for the medicine in children under 6.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => do-not-supply-phenergan-to-children-under-6-manufacturer-warns
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-21 09:54:51
[post_modified_gmt] => 2024-11-20 22:54:51
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28164
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Do not supply Phenergan to children under 6, manufacturer warns
[title] => Do not supply Phenergan to children under 6, manufacturer warns
[href] => https://www.australianpharmacist.com.au/do-not-supply-phenergan-to-children-under-6-manufacturer-warns/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28167
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28313
[post_author] => 3410
[post_date] => 2024-11-25 12:46:22
[post_date_gmt] => 2024-11-25 01:46:22
[post_content] => These oft-used medicines have become the analgesia of choice for many prescribers. But care should be taken before prescribing gabapentinoids to certain patients.
Gabapentinoid medicines are widely prescribed in Australia. Considered a safer alternative to opioids for neuropathic pain, there was an 8-fold increase in prescriptions for gabapentinoids from 2012 to 2018 – with 1 in 7 Australians aged 80 and older prescribed a gabapentinoid.
[caption id="attachment_28316" align="aligncenter" width="1280"]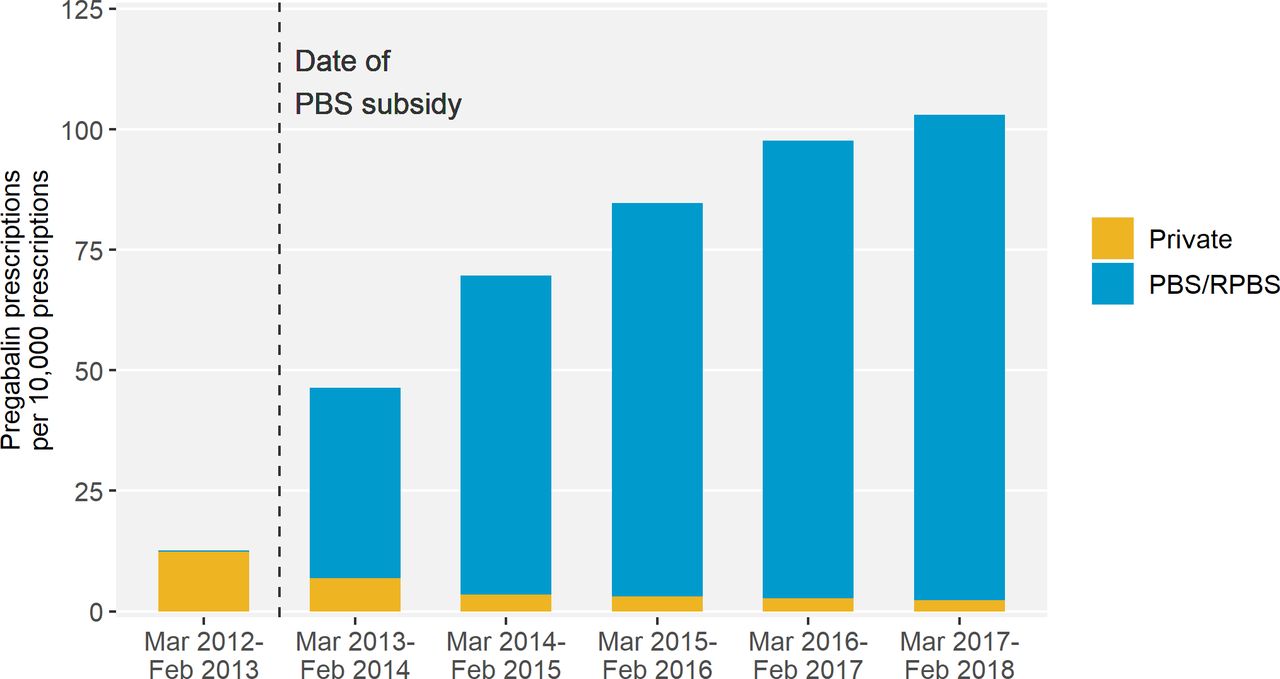 Source – Pregabalin prescribing patterns in Australian general practice, 2012–2018: a cross-sectional study[/caption]
But a new study from Monash University researchers, including pharmacists Miriam Leung and Professor Simon Bell FPS, found that harm can be caused within 2 months of initiation.
Over a 5-year period, the researchers analysed data for 28,293 patients in Victoria who experienced hip fractures.
‘Our research found that patients who were recently dispensed either pregabalin or gabapentin had 30% higher odds of experiencing a hip fracture,’ Prof Bell told Australian Pharmacist.
Source – Pregabalin prescribing patterns in Australian general practice, 2012–2018: a cross-sectional study[/caption]
But a new study from Monash University researchers, including pharmacists Miriam Leung and Professor Simon Bell FPS, found that harm can be caused within 2 months of initiation.
Over a 5-year period, the researchers analysed data for 28,293 patients in Victoria who experienced hip fractures.
‘Our research found that patients who were recently dispensed either pregabalin or gabapentin had 30% higher odds of experiencing a hip fracture,’ Prof Bell told Australian Pharmacist.
Who is most at risk?
The link between gabapentinoid use and hip fractures existed across different age groups.
However, the risk of hip fracture associated with gabapentinoid medicines was highest in patients who were frail or had renal impairment, said Prof Bell.
‘Frail older people are prone to falls and fractures,’ he said. ‘One in 25 adults aged 80 years and older experience a hip fracture each year.’
The impact of these incidents can be fatal.
‘Around one in four people who experience a hip fracture die within 12 months,’ said Prof Bell.
How should pharmacists assess and manage falls risk?
For certain neuropathic pain conditions such as postherpetic neuralgia, diabetic neuropathy, and mixed or post-traumatic neuropathy, gabapentinoids such as pregabalin or gabapentin can provide effective relief.
However, while approved by the Australian Therapeutic Goods Administration for refractory focal (partial) epilepsy and neuropathic pain, gabapentin and pregabalin are often prescribed off label – with limited evidence to support efficacy for off-label indications.
In patients who are likely to see some benefit of therapy, pharmacists should advise patients how to minimise risk before dispensing these medicines.
‘The risk of falls is highest at the start of treatment,’ said Prof Bell.
‘Therefore, it’s important that pharmacists and other clinicians advise on strategies to minimise falls risk at this time. This could include avoidance of other falls-risk increasing substances such as alcohol.’
Evaluating what other medicines at-risk patients are prescribed is also an important strategy for preventing harm.
‘It’s known that gabapentinoids can cause side-effects such as drowsiness, sedation and dizziness,’ said Prof Bell.
‘These side-effects may increase the risk of falls, particularly if gabapentinoids are co-administrated with other psychotropic or cardiovascular falls risk medications.’
What impact can dose have on falls risk?
Given risk is highest at the outset of treatment, the starting dose of gabapentinoids can also have an impact on the likelihood of falls.
‘It’s advisable that patients start with a low dose and titrate slowly,’ said Prof Bell. ‘This particularly applies to people who are frail or have renal impairment.’
When is a discussion with the prescriber warranted?
The ongoing need for gabapentinoid treatment for neuropathic pain should be reviewed regularly, said Prof Bell.
‘If patients do not experience benefit after an adequate trial of treatment, then gradual discontinuation may be warranted,’ he said.
However, it’s important to advise people who take a gabapentinoid medicine that they shouldn’t stop taking their medication without first speaking with their prescriber or pharmacist first.
‘Stopping gabapentinoid medications abruptly can cause withdrawal symptoms,’ Prof Bell added.
[post_title] => Neuropathic pain medicines can increase the risk of falls
[post_excerpt] =>
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => neuropathic-pain-medicines-can-increase-the-risk-of-falls
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-25 15:20:38
[post_modified_gmt] => 2024-11-25 04:20:38
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28313
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Neuropathic pain medicines can increase the risk of falls
[title] => Neuropathic pain medicines can increase the risk of falls
[href] => https://www.australianpharmacist.com.au/neuropathic-pain-medicines-can-increase-the-risk-of-falls/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28319
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28263
[post_author] => 3410
[post_date] => 2024-11-20 13:37:02
[post_date_gmt] => 2024-11-20 02:37:02
[post_content] => Australia’s understanding and adoption of Quality Use of Medicines (QUM) principles across general practice and primary care has led to overall improvements in medicine use, such as curtailing high-dose use of proton pump inhibitors.
But the challenge has since changed, with Australians living longer – resulting in an older, sicker population who uses more medicines, said Professor Libby Roughead – Director of the QUM and Pharmacy Research Centre at the University of South Australia.
‘Now the game is to say, how do we go forward when we’ve got a frail older population, and lots of specialty medicine? she asked.
This is the question a panel of experts sought to answer at the National Medicines Symposium 2024 yesterday (19 November).
Be wary of using ‘wonder drugs’ in older patients
When clinical trials are conducted on new medicines, they’re not tested in the over 65 age group, said Steve Waller, Senior Advisor, Medication without Harm, Australian Commission on Safety and Quality in Health Care.
[caption id="attachment_28267" align="alignnone" width="800"] National Medicines Symposium 2024 speakers (L to R): Steve Waller, Professor Jennifer Martin, Professor Libby Roughead, Tegan Taylor[/caption]
‘That creates complications, because we often don’t know what the impact in that older age group is … and pharmaceutical companies don’t have that information when they’re making an application for a new drug to be listed with the TGA [Therapeutic Goods Administration] and PBS [Pharmaceutical Benefits Scheme],’ he said.
Healthcare professionals must have awareness of the limitations of the data, thinks Professor Jennifer Martin, clinical pharmacologist and president of the Royal Australian College of Physicians.
‘Often, I say to people “why are you using a statin in [an older] population? We know the life expectancy when you go to a nursing home is less than 2 years, and you have to be on this drug at this dose for 5 years just to see a small reduction in a composite end point”,’ she said.
Healthcare professionals should rely on Australia’s ‘good sources of objective information’ such as Therapeutic Guidelines and the Australian Medicines Handbook, said Prof Roughead.
But more work needs to be done on increasing uptake of non-pharmacological interventions that are suitable for many conditions, including art therapy, music therapy, exercise and diet.
‘We know compassion practices are really helpful in some of the hard-to-treat conditions [such as] pain and depression, so we need to get better at involving the whole therapeutic armamentarium,’ she said. ‘The first definition of QUM is judicious selection of management options.’
National Medicines Symposium 2024 speakers (L to R): Steve Waller, Professor Jennifer Martin, Professor Libby Roughead, Tegan Taylor[/caption]
‘That creates complications, because we often don’t know what the impact in that older age group is … and pharmaceutical companies don’t have that information when they’re making an application for a new drug to be listed with the TGA [Therapeutic Goods Administration] and PBS [Pharmaceutical Benefits Scheme],’ he said.
Healthcare professionals must have awareness of the limitations of the data, thinks Professor Jennifer Martin, clinical pharmacologist and president of the Royal Australian College of Physicians.
‘Often, I say to people “why are you using a statin in [an older] population? We know the life expectancy when you go to a nursing home is less than 2 years, and you have to be on this drug at this dose for 5 years just to see a small reduction in a composite end point”,’ she said.
Healthcare professionals should rely on Australia’s ‘good sources of objective information’ such as Therapeutic Guidelines and the Australian Medicines Handbook, said Prof Roughead.
But more work needs to be done on increasing uptake of non-pharmacological interventions that are suitable for many conditions, including art therapy, music therapy, exercise and diet.
‘We know compassion practices are really helpful in some of the hard-to-treat conditions [such as] pain and depression, so we need to get better at involving the whole therapeutic armamentarium,’ she said. ‘The first definition of QUM is judicious selection of management options.’
Involve older patients in deprescribing decisions
Doctors, pharmacists, family members and carers typically talk among themselves about an older patient's medicine regimen. But it’s the patient they need to focus on, thinks Prof Martin.
‘When you talk to an older person, they will typically say “I don’t know why they started those pills” or “I don’t think I was supposed to be on them long-term, but no one stopped them, so I just kept taking them”,’ she said.
‘So, come back to the patient and ask, “Why are you taking these medications? What are your goals of care? Do you want pain relief? What are you looking for?”’
As patients reach their final chapter, many are just after quality of life – which doesn’t necessarily entail losing cognitive function through heavy use of opioids.
‘Opioids may play some role in pain, but they certainly take away a lot of the quality of life for older people,’ said Prof Martin. ‘It’s not until you spend time talking to the person that you find out they actually want to be very sharp; they think they can cope with their pain by other measures, and we can probably reduce some of their opioids.’
Warranted distrust in medicines and healthcare needs to be built back up
While we live in an age where misinformation is rife, some of it stems from the health system and pharma model, said Prof Martin.
‘For example, we know with gabapentin, which some people use for pain, most of the information that got onto the market was fraudulent,’ she said. ‘[There] was then a big investigation, with lawsuits still ongoing.’
The same goes for opioids, ineffective for many of the conditions they are prescribed for – particularly chronic pain.
‘The public are looking at their health providers saying, “We now know this is misinformation, but you prescribed this”, so we’ve lost a bit of engagement with our community,’ said Prof Martin.
With many patients with chronic pain on high doses of opioids that are not treating their conditions and impairing their quality of life, Prof Martin thinks the healthcare sector has ‘something to answer for’.
‘That misinformation is coming from industry and from the fact that we’re too busy to actually go back to their source material,’ she said.
The good news is that opioid deaths have decreased over the last 5 years in Australia, thanks to tighter prescribing regulations and better resources such as the Opioid Analgesic Stewardship in Acute Pain Clinical Care Standard, said Mr Waller.
Work on state formularies has also reduced the number of opioids that people can prescribe, said Prof Martin.
‘It has helped to get that conversation going of “Why do you need to have access to 10 different opioids in an in-patient setting?” and “Why do you need all these different concentrations?”’ she said.
However, more changes in practice are required to ensure that trend continues in the right direction, said Mr Waller.
‘We need to stop using opioids for chronic pain,’ he said. ‘There’s limited to no evidence to suggest that they work, and we need to be very judicious about our use of modified-release opioid analgesics.’
Yet as that work is done, it’s crucial to remember that these patients are suffering and compassion should be brought to the encounter – rather than simply saying ‘you can’t have that’, said Prof Roughead.
‘It’s not just ceasing a medicine. It’s ceasing a medicine and starting other things that you might need to help you be well, whether it be an exercise program or psychological services,’ she said.
Pharmacists can bridge communication and healthcare gaps in RACFs
With the Aged Care On-site Pharmacist (ACOP) program kicking off on 1 July 2024, pharmacists can improve the approach to healthcare by simply getting to know people – a skill well-honed by pharmacists in other settings, said Prof Roughead.
This includes understanding patient preferences and non-pharmacological activities that might support them.
‘If we can build a system where we can create relationships, particularly in a virtual world … we’re all going to be safer and we’re all going to feel better,’ she said.
‘That’s got to be the strength of an embedded pharmacist in aged care, that day-to-day knowledge of what the patient’s likes and dislikes are and how they’ve been managed over a continuum, as opposed to a visit that might happen once a year,’ added Mr Waller.
As the custodian of the pharmacy profession’s Professional Practice Standards and an education and training provider, PSA has continued to invest and embark into practice support training and education for pharmacists to become ACOP credentialed, said PSA National President Associated Professor Fei Sim.
The training covers all elements of this role – from professionalism, to understanding the governance of an RACF, collaborative practice, providing person-centred medication management and working within a multidisciplinary team to improve the safe and quality use of medicines.
‘Pharmacists undertaking the training program would then acquire the necessary credentials, qualifications and skill set to be able to undertake the role as an aged care on-site pharmacist,’ she said.
‘We’re also providing ongoing resources and clinical updates for credentialed pharmacists so they can be kept up to date with their knowledge and skills to undertake the role.’
With any new areas of practice, there is a great need for mentoring and networking for like-minded pharmacists who work in the same area to forge bonds, said A/Prof Sim. ‘That’s why PSA created the Consultant Pharmacists CSI group [and] an annual Consultant Pharmacist Conference, focusing on supporting and meeting the learning needs of credentialed pharmacists.’
[post_title] => Giving a voice back to elderly patients
[post_excerpt] => Yesterday’s National Medicine Symposium delivered a stark critique of how our health system is failing older patients – and how to fix it.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => giving-a-voice-back-to-elderly-patients
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-20 15:44:59
[post_modified_gmt] => 2024-11-20 04:44:59
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28263
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Giving a voice back to elderly patients
[title] => Giving a voice back to elderly patients
[href] => https://www.australianpharmacist.com.au/giving-a-voice-back-to-elderly-patients/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28266
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28254
[post_author] => 3410
[post_date] => 2024-11-18 13:05:58
[post_date_gmt] => 2024-11-18 02:05:58
[post_content] => Mpox cases are surging in Australia. An expert reveals how pharmacists can address the rising spread.
When mpox was first reported in Australia in May 2022, case numbers remained relatively low for the better part of 2 years.
However, in 2024 there has been a significant spike in case numbers in several Australian states and territories, with New South Wales, Victoria and Western Australia all seeing rising locally acquired notifications.
In September, it was reported that mpox cases grew a staggering 570% since July 2024 –with over 724 cases recorded this year. Yet vaccination rates remain low.
Meanwhile, cases of clade Ib – which has a much higher fatality rate than clade IIb strain spreading in Australia – have been detected in numerous countries around the world, most recently the United States. The worldwide spread of the new clade led the World Health Organisation to declare the mpox outbreak a public health emergency of international concern.
At this stage, pharmacists can only administer the mpox vaccine in Victoria and the Northern Territory.
However, pharmacists in all jurisdictions have an essential role in raising awareness of vaccine eligibility and dosing schedule, when to get vaccinated and where to get tested – all of which can help to bring down rising case numbers.
Watch the video below to hear sexual health expert Dr Tom Morley explain how pharmacists can go about this in a culturally safe way.
https://www.youtube.com/watch?v=ZPzbadkq8sM
[post_title] => Curbing the spread as mpox cases skyrocket
[post_excerpt] => Mpox cases are surging both in Australia and around the world. An expert reveals how pharmacists can address the rising spread.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => curbing-the-spread-as-mpox-cases-skyrocket
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-18 15:16:33
[post_modified_gmt] => 2024-11-18 04:16:33
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28254
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Curbing the spread as mpox cases skyrocket
[title] => Curbing the spread as mpox cases skyrocket
[href] => https://www.australianpharmacist.com.au/curbing-the-spread-as-mpox-cases-skyrocket/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28257
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28190
[post_author] => 46
[post_date] => 2024-11-18 09:28:17
[post_date_gmt] => 2024-11-17 22:28:17
[post_content] => Constipation can be an embarrassing topic to discuss with your patients. But irregular bowel movements can not only be uncomfortable, but can lead to other health conditions and severely impact a patient’s quality of life.
[caption id="attachment_28205" align="alignright" width="150"] This CPD activity is sponsored by Reckitt. All content is the true, accurate and independent opinion of the speakers and the views expressed are entirely their own.[/caption]
Constipation is a common problem in the community,1 that can significantly impact quality of life if not properly managed.2 It’s also a common reason for primary care visits and referrals to gastroenterologists.3 Unfortunately, many patients are choosing laxatives without the help and advice of a health professional1 so may be choosing products that don’t work effectively5 or choosing to use laxatives when addressing dietary, lifestyle or medicine regimens may be the most appropriate course of action. In this CPD accredited podcast, listen to Priceline Health Services Manager Brett Macfarlane and Senior Clinical Pharmacist – Gastroenterology at the Royal Melbourne Hospital Stephanie Dimovski discuss the problem of constipation and how pharmacists can assist patients in managing this condition. They will address the importance of identifying whether insufficient fibre and fluid intake may be contributing and whether making dietary and exercise recommendations is enough to restore normal bowel habits.
This CPD activity is sponsored by Reckitt. All content is the true, accurate and independent opinion of the speakers and the views expressed are entirely their own.[/caption]
Constipation is a common problem in the community,1 that can significantly impact quality of life if not properly managed.2 It’s also a common reason for primary care visits and referrals to gastroenterologists.3 Unfortunately, many patients are choosing laxatives without the help and advice of a health professional1 so may be choosing products that don’t work effectively5 or choosing to use laxatives when addressing dietary, lifestyle or medicine regimens may be the most appropriate course of action. In this CPD accredited podcast, listen to Priceline Health Services Manager Brett Macfarlane and Senior Clinical Pharmacist – Gastroenterology at the Royal Melbourne Hospital Stephanie Dimovski discuss the problem of constipation and how pharmacists can assist patients in managing this condition. They will address the importance of identifying whether insufficient fibre and fluid intake may be contributing and whether making dietary and exercise recommendations is enough to restore normal bowel habits.
After reading this article, pharmacists should be able to:
|
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28164
[post_author] => 3410
[post_date] => 2024-11-13 12:50:58
[post_date_gmt] => 2024-11-13 01:50:58
[post_content] => The Therapeutic Goods Administration (TGA) has worked with Phenergan manufacturer Sanofi to develop a new contraindication for the medicine in children under 6.
The decision to restrict use of the medicine in this age cohort – commonly used to treat allergies, travel sickness and nausea – is based on a thorough evaluation of new scientific evidence that the risks outweigh the benefits, a spokesperson for Sanofi told Australian Pharmacist.
‘Following recent evaluations made by Sanofi Consumer Healthcare Pty Ltd, including a benefit-risk assessment, the research has shown a causal association between promethazine and safety concerns,’ said this spokesperson.
The sponsor-initiated update was prompted by advice from the TGA Advisory Committee on Medicines (ACM) – first-generation oral sedating antihistamines – do not use in children, said a spokesperson from the TGA.
‘Further review by the sponsor of cumulative safety data in children 2 to 5 years of age demonstrated sufficient evidence of a causal association between promethazine and psychiatric and central nervous system adverse events in this age group,’ the TGA spokesperson told AP.
The contraindication comes after Medsafe, the New Zealand Medicines and Medical Devices Safety Authority, moved to contraindicate the use of the medicine in children under 6 due to the potential for fatal respiratory depression, psychiatric and central nervous system (CNS) events.
AP understands that the contraindication will affect other products. A spokesperson for AFT said a variation has been submitted to update the product information and label on Allersoothe Elixir with a change to the age indication from children 2 years and older to children 6 years and older. This submission is pending approval.
Will the packaging change?
Not immediately.
New labels for promethazine-containing products will be rolled out in 2025 due to production and logistics lead times, said the Sanofi spokesperson.
‘No immediate action is required regarding current stock. There is no need to set aside existing medications, as this communication does not constitute a recall,’ said the spokesperson. ‘Similarly, the revised labels do not create any changes in the ordering process.
The product information for Phenergan has been updated and is available here.
What should pharmacists do if they get a Phenergan script for an 18 month old infant?
The use of promethazine in children under 6 years of age is now both contraindicated and off label, said Peter Guthrey MPS, PSA Senior Pharmacist – strategic policy.
‘This means that if you choose to dispense, both the prescriber and dispenser carry the full indemnity risk, and you need to get the patient to provide informed consent,’ he said.
Should a parent present with a script for promethazine for use in a child under 6 years of age, pharmacists should contact the prescriber to discuss the risks and benefits, noting that it's contraindicated.
Is there any situation where it would be appropriate to dispense Phenergan to a young child?
It would need to be a pretty compelling case, where the benefit to a child outweighed the risk of respiratory depression, psychiatric or CNS events, said Mr Guthrey.
‘Given it’s a documented contraindication, it'd be pretty hard to demonstrate the medicine is ‘‘safe and therapeutically appropriate’’,’ he said.
‘It is going to be difficult to find a situation where supply is clinically justified and pharmacists have met their obligations to patient safety.’
What about prescribing Phenergan as a Schedule 3 medicine?
If a parent requests promethazine as a Schedule 3 medicine for someone under the age of 6 years, generally alternate products or advice for treatment should be provided following a discussion.
‘While a pharmacist prescribing promethazine as a Pharmacist Only Medicine is lawful for children aged 2-5 years, it is still contraindicated,’ said Mr Guthrey. ‘There would be very few, if any, situations where prescribing the medicine where contraindicated would be warranted.’
What about phenylephrine?
There are some combination phenylephrine products indicated for children under 6 years of age for nasal congestion. However, there is plenty of evidence showing that oral phenylephrine products are ineffective as a nasal decongestant.
In fact, the United States Food and Drug Administration (FDA) recently announced it will move to ban oral phenylephrine products because they simply don't work.
‘Based on our review of available data, and consistent with the advice of the advisory committee, we are taking this next step in the process to propose removing oral phenylephrine because it is not effective as a nasal decongestant,’ said Patrizia Cavazzoni, M.D., director of the FDA’s Center for Drug Evaluation and Research.
While a spokesperson for the TGA told Australian Pharmacist back in July that there are ‘no plans’ to review the effectiveness of oral phenylephrine, it will continue to monitor the outcomes of the FDA review.
What advice should pharmacists provide?
For children with allergies, non-sedating antihistamines are first line.
The best thing parents can do when a child under 6 years of age has cough or cold symptoms is to wait it out, with a review by a medical practitioner when appropriate.
‘It's about reassurance to parents that the cough in itself isn't harmful, and that kids don’t always need medicines for a cold – they need time and supportive therapy,’ said Mr Guthrey.
It’s important that pharmacists give parents confidence that they're doing the right thing by not treating the cough, and providing symptomatic relief for fever and chills – ensuring they are appropriately counselled on when review by a medical practitioner may be appropriate.
For more information, refer to the Australian Pharmaceutical Formulary and Handbook treatment guidelines on:
[post_title] => Do not supply Phenergan to children under 6, manufacturer warns
[post_excerpt] => The TGA has worked with Phenergan manufacturer Sanofi to develop a new contraindication for the medicine in children under 6.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => do-not-supply-phenergan-to-children-under-6-manufacturer-warns
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-21 09:54:51
[post_modified_gmt] => 2024-11-20 22:54:51
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28164
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Do not supply Phenergan to children under 6, manufacturer warns
[title] => Do not supply Phenergan to children under 6, manufacturer warns
[href] => https://www.australianpharmacist.com.au/do-not-supply-phenergan-to-children-under-6-manufacturer-warns/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28167
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28313
[post_author] => 3410
[post_date] => 2024-11-25 12:46:22
[post_date_gmt] => 2024-11-25 01:46:22
[post_content] => These oft-used medicines have become the analgesia of choice for many prescribers. But care should be taken before prescribing gabapentinoids to certain patients.
Gabapentinoid medicines are widely prescribed in Australia. Considered a safer alternative to opioids for neuropathic pain, there was an 8-fold increase in prescriptions for gabapentinoids from 2012 to 2018 – with 1 in 7 Australians aged 80 and older prescribed a gabapentinoid.
[caption id="attachment_28316" align="aligncenter" width="1280"]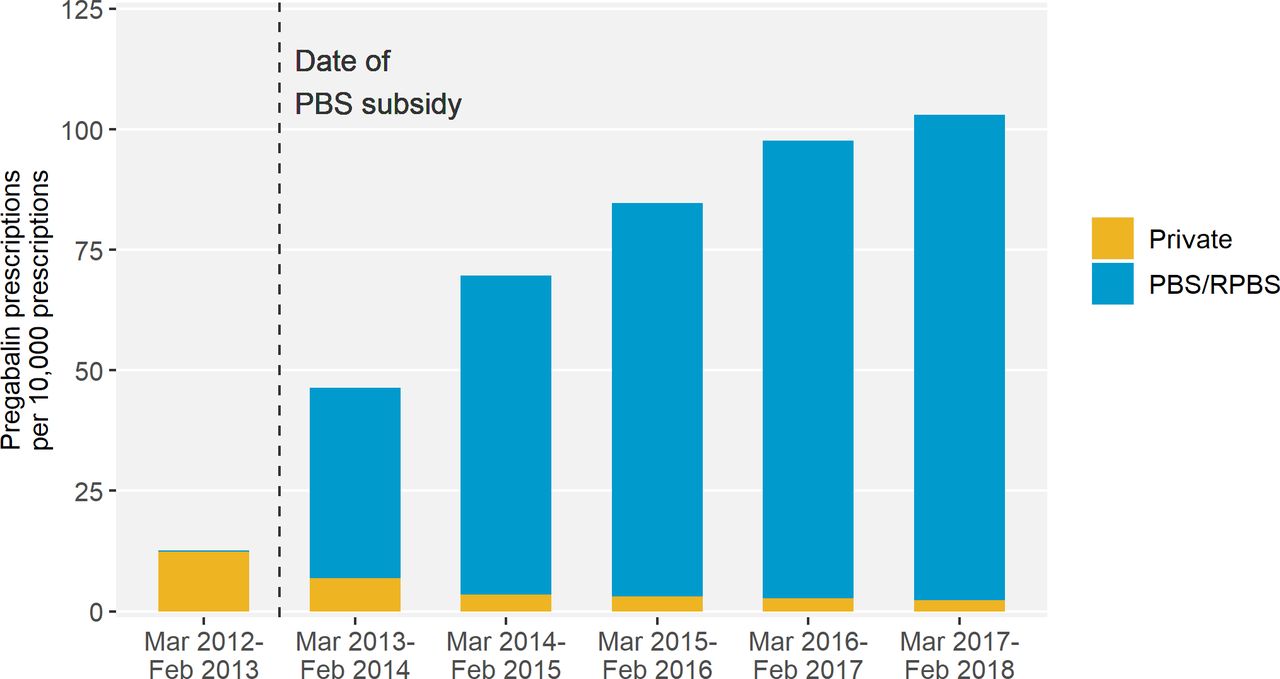 Source – Pregabalin prescribing patterns in Australian general practice, 2012–2018: a cross-sectional study[/caption]
But a new study from Monash University researchers, including pharmacists Miriam Leung and Professor Simon Bell FPS, found that harm can be caused within 2 months of initiation.
Over a 5-year period, the researchers analysed data for 28,293 patients in Victoria who experienced hip fractures.
‘Our research found that patients who were recently dispensed either pregabalin or gabapentin had 30% higher odds of experiencing a hip fracture,’ Prof Bell told Australian Pharmacist.
Source – Pregabalin prescribing patterns in Australian general practice, 2012–2018: a cross-sectional study[/caption]
But a new study from Monash University researchers, including pharmacists Miriam Leung and Professor Simon Bell FPS, found that harm can be caused within 2 months of initiation.
Over a 5-year period, the researchers analysed data for 28,293 patients in Victoria who experienced hip fractures.
‘Our research found that patients who were recently dispensed either pregabalin or gabapentin had 30% higher odds of experiencing a hip fracture,’ Prof Bell told Australian Pharmacist.
Who is most at risk?
The link between gabapentinoid use and hip fractures existed across different age groups.
However, the risk of hip fracture associated with gabapentinoid medicines was highest in patients who were frail or had renal impairment, said Prof Bell.
‘Frail older people are prone to falls and fractures,’ he said. ‘One in 25 adults aged 80 years and older experience a hip fracture each year.’
The impact of these incidents can be fatal.
‘Around one in four people who experience a hip fracture die within 12 months,’ said Prof Bell.
How should pharmacists assess and manage falls risk?
For certain neuropathic pain conditions such as postherpetic neuralgia, diabetic neuropathy, and mixed or post-traumatic neuropathy, gabapentinoids such as pregabalin or gabapentin can provide effective relief.
However, while approved by the Australian Therapeutic Goods Administration for refractory focal (partial) epilepsy and neuropathic pain, gabapentin and pregabalin are often prescribed off label – with limited evidence to support efficacy for off-label indications.
In patients who are likely to see some benefit of therapy, pharmacists should advise patients how to minimise risk before dispensing these medicines.
‘The risk of falls is highest at the start of treatment,’ said Prof Bell.
‘Therefore, it’s important that pharmacists and other clinicians advise on strategies to minimise falls risk at this time. This could include avoidance of other falls-risk increasing substances such as alcohol.’
Evaluating what other medicines at-risk patients are prescribed is also an important strategy for preventing harm.
‘It’s known that gabapentinoids can cause side-effects such as drowsiness, sedation and dizziness,’ said Prof Bell.
‘These side-effects may increase the risk of falls, particularly if gabapentinoids are co-administrated with other psychotropic or cardiovascular falls risk medications.’
What impact can dose have on falls risk?
Given risk is highest at the outset of treatment, the starting dose of gabapentinoids can also have an impact on the likelihood of falls.
‘It’s advisable that patients start with a low dose and titrate slowly,’ said Prof Bell. ‘This particularly applies to people who are frail or have renal impairment.’
When is a discussion with the prescriber warranted?
The ongoing need for gabapentinoid treatment for neuropathic pain should be reviewed regularly, said Prof Bell.
‘If patients do not experience benefit after an adequate trial of treatment, then gradual discontinuation may be warranted,’ he said.
However, it’s important to advise people who take a gabapentinoid medicine that they shouldn’t stop taking their medication without first speaking with their prescriber or pharmacist first.
‘Stopping gabapentinoid medications abruptly can cause withdrawal symptoms,’ Prof Bell added.
[post_title] => Neuropathic pain medicines can increase the risk of falls
[post_excerpt] =>
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => neuropathic-pain-medicines-can-increase-the-risk-of-falls
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-25 15:20:38
[post_modified_gmt] => 2024-11-25 04:20:38
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28313
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Neuropathic pain medicines can increase the risk of falls
[title] => Neuropathic pain medicines can increase the risk of falls
[href] => https://www.australianpharmacist.com.au/neuropathic-pain-medicines-can-increase-the-risk-of-falls/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28319
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28263
[post_author] => 3410
[post_date] => 2024-11-20 13:37:02
[post_date_gmt] => 2024-11-20 02:37:02
[post_content] => Australia’s understanding and adoption of Quality Use of Medicines (QUM) principles across general practice and primary care has led to overall improvements in medicine use, such as curtailing high-dose use of proton pump inhibitors.
But the challenge has since changed, with Australians living longer – resulting in an older, sicker population who uses more medicines, said Professor Libby Roughead – Director of the QUM and Pharmacy Research Centre at the University of South Australia.
‘Now the game is to say, how do we go forward when we’ve got a frail older population, and lots of specialty medicine? she asked.
This is the question a panel of experts sought to answer at the National Medicines Symposium 2024 yesterday (19 November).
Be wary of using ‘wonder drugs’ in older patients
When clinical trials are conducted on new medicines, they’re not tested in the over 65 age group, said Steve Waller, Senior Advisor, Medication without Harm, Australian Commission on Safety and Quality in Health Care.
[caption id="attachment_28267" align="alignnone" width="800"] National Medicines Symposium 2024 speakers (L to R): Steve Waller, Professor Jennifer Martin, Professor Libby Roughead, Tegan Taylor[/caption]
‘That creates complications, because we often don’t know what the impact in that older age group is … and pharmaceutical companies don’t have that information when they’re making an application for a new drug to be listed with the TGA [Therapeutic Goods Administration] and PBS [Pharmaceutical Benefits Scheme],’ he said.
Healthcare professionals must have awareness of the limitations of the data, thinks Professor Jennifer Martin, clinical pharmacologist and president of the Royal Australian College of Physicians.
‘Often, I say to people “why are you using a statin in [an older] population? We know the life expectancy when you go to a nursing home is less than 2 years, and you have to be on this drug at this dose for 5 years just to see a small reduction in a composite end point”,’ she said.
Healthcare professionals should rely on Australia’s ‘good sources of objective information’ such as Therapeutic Guidelines and the Australian Medicines Handbook, said Prof Roughead.
But more work needs to be done on increasing uptake of non-pharmacological interventions that are suitable for many conditions, including art therapy, music therapy, exercise and diet.
‘We know compassion practices are really helpful in some of the hard-to-treat conditions [such as] pain and depression, so we need to get better at involving the whole therapeutic armamentarium,’ she said. ‘The first definition of QUM is judicious selection of management options.’
National Medicines Symposium 2024 speakers (L to R): Steve Waller, Professor Jennifer Martin, Professor Libby Roughead, Tegan Taylor[/caption]
‘That creates complications, because we often don’t know what the impact in that older age group is … and pharmaceutical companies don’t have that information when they’re making an application for a new drug to be listed with the TGA [Therapeutic Goods Administration] and PBS [Pharmaceutical Benefits Scheme],’ he said.
Healthcare professionals must have awareness of the limitations of the data, thinks Professor Jennifer Martin, clinical pharmacologist and president of the Royal Australian College of Physicians.
‘Often, I say to people “why are you using a statin in [an older] population? We know the life expectancy when you go to a nursing home is less than 2 years, and you have to be on this drug at this dose for 5 years just to see a small reduction in a composite end point”,’ she said.
Healthcare professionals should rely on Australia’s ‘good sources of objective information’ such as Therapeutic Guidelines and the Australian Medicines Handbook, said Prof Roughead.
But more work needs to be done on increasing uptake of non-pharmacological interventions that are suitable for many conditions, including art therapy, music therapy, exercise and diet.
‘We know compassion practices are really helpful in some of the hard-to-treat conditions [such as] pain and depression, so we need to get better at involving the whole therapeutic armamentarium,’ she said. ‘The first definition of QUM is judicious selection of management options.’
Involve older patients in deprescribing decisions
Doctors, pharmacists, family members and carers typically talk among themselves about an older patient's medicine regimen. But it’s the patient they need to focus on, thinks Prof Martin.
‘When you talk to an older person, they will typically say “I don’t know why they started those pills” or “I don’t think I was supposed to be on them long-term, but no one stopped them, so I just kept taking them”,’ she said.
‘So, come back to the patient and ask, “Why are you taking these medications? What are your goals of care? Do you want pain relief? What are you looking for?”’
As patients reach their final chapter, many are just after quality of life – which doesn’t necessarily entail losing cognitive function through heavy use of opioids.
‘Opioids may play some role in pain, but they certainly take away a lot of the quality of life for older people,’ said Prof Martin. ‘It’s not until you spend time talking to the person that you find out they actually want to be very sharp; they think they can cope with their pain by other measures, and we can probably reduce some of their opioids.’
Warranted distrust in medicines and healthcare needs to be built back up
While we live in an age where misinformation is rife, some of it stems from the health system and pharma model, said Prof Martin.
‘For example, we know with gabapentin, which some people use for pain, most of the information that got onto the market was fraudulent,’ she said. ‘[There] was then a big investigation, with lawsuits still ongoing.’
The same goes for opioids, ineffective for many of the conditions they are prescribed for – particularly chronic pain.
‘The public are looking at their health providers saying, “We now know this is misinformation, but you prescribed this”, so we’ve lost a bit of engagement with our community,’ said Prof Martin.
With many patients with chronic pain on high doses of opioids that are not treating their conditions and impairing their quality of life, Prof Martin thinks the healthcare sector has ‘something to answer for’.
‘That misinformation is coming from industry and from the fact that we’re too busy to actually go back to their source material,’ she said.
The good news is that opioid deaths have decreased over the last 5 years in Australia, thanks to tighter prescribing regulations and better resources such as the Opioid Analgesic Stewardship in Acute Pain Clinical Care Standard, said Mr Waller.
Work on state formularies has also reduced the number of opioids that people can prescribe, said Prof Martin.
‘It has helped to get that conversation going of “Why do you need to have access to 10 different opioids in an in-patient setting?” and “Why do you need all these different concentrations?”’ she said.
However, more changes in practice are required to ensure that trend continues in the right direction, said Mr Waller.
‘We need to stop using opioids for chronic pain,’ he said. ‘There’s limited to no evidence to suggest that they work, and we need to be very judicious about our use of modified-release opioid analgesics.’
Yet as that work is done, it’s crucial to remember that these patients are suffering and compassion should be brought to the encounter – rather than simply saying ‘you can’t have that’, said Prof Roughead.
‘It’s not just ceasing a medicine. It’s ceasing a medicine and starting other things that you might need to help you be well, whether it be an exercise program or psychological services,’ she said.
Pharmacists can bridge communication and healthcare gaps in RACFs
With the Aged Care On-site Pharmacist (ACOP) program kicking off on 1 July 2024, pharmacists can improve the approach to healthcare by simply getting to know people – a skill well-honed by pharmacists in other settings, said Prof Roughead.
This includes understanding patient preferences and non-pharmacological activities that might support them.
‘If we can build a system where we can create relationships, particularly in a virtual world … we’re all going to be safer and we’re all going to feel better,’ she said.
‘That’s got to be the strength of an embedded pharmacist in aged care, that day-to-day knowledge of what the patient’s likes and dislikes are and how they’ve been managed over a continuum, as opposed to a visit that might happen once a year,’ added Mr Waller.
As the custodian of the pharmacy profession’s Professional Practice Standards and an education and training provider, PSA has continued to invest and embark into practice support training and education for pharmacists to become ACOP credentialed, said PSA National President Associated Professor Fei Sim.
The training covers all elements of this role – from professionalism, to understanding the governance of an RACF, collaborative practice, providing person-centred medication management and working within a multidisciplinary team to improve the safe and quality use of medicines.
‘Pharmacists undertaking the training program would then acquire the necessary credentials, qualifications and skill set to be able to undertake the role as an aged care on-site pharmacist,’ she said.
‘We’re also providing ongoing resources and clinical updates for credentialed pharmacists so they can be kept up to date with their knowledge and skills to undertake the role.’
With any new areas of practice, there is a great need for mentoring and networking for like-minded pharmacists who work in the same area to forge bonds, said A/Prof Sim. ‘That’s why PSA created the Consultant Pharmacists CSI group [and] an annual Consultant Pharmacist Conference, focusing on supporting and meeting the learning needs of credentialed pharmacists.’
[post_title] => Giving a voice back to elderly patients
[post_excerpt] => Yesterday’s National Medicine Symposium delivered a stark critique of how our health system is failing older patients – and how to fix it.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => giving-a-voice-back-to-elderly-patients
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-20 15:44:59
[post_modified_gmt] => 2024-11-20 04:44:59
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28263
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Giving a voice back to elderly patients
[title] => Giving a voice back to elderly patients
[href] => https://www.australianpharmacist.com.au/giving-a-voice-back-to-elderly-patients/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28266
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28254
[post_author] => 3410
[post_date] => 2024-11-18 13:05:58
[post_date_gmt] => 2024-11-18 02:05:58
[post_content] => Mpox cases are surging in Australia. An expert reveals how pharmacists can address the rising spread.
When mpox was first reported in Australia in May 2022, case numbers remained relatively low for the better part of 2 years.
However, in 2024 there has been a significant spike in case numbers in several Australian states and territories, with New South Wales, Victoria and Western Australia all seeing rising locally acquired notifications.
In September, it was reported that mpox cases grew a staggering 570% since July 2024 –with over 724 cases recorded this year. Yet vaccination rates remain low.
Meanwhile, cases of clade Ib – which has a much higher fatality rate than clade IIb strain spreading in Australia – have been detected in numerous countries around the world, most recently the United States. The worldwide spread of the new clade led the World Health Organisation to declare the mpox outbreak a public health emergency of international concern.
At this stage, pharmacists can only administer the mpox vaccine in Victoria and the Northern Territory.
However, pharmacists in all jurisdictions have an essential role in raising awareness of vaccine eligibility and dosing schedule, when to get vaccinated and where to get tested – all of which can help to bring down rising case numbers.
Watch the video below to hear sexual health expert Dr Tom Morley explain how pharmacists can go about this in a culturally safe way.
https://www.youtube.com/watch?v=ZPzbadkq8sM
[post_title] => Curbing the spread as mpox cases skyrocket
[post_excerpt] => Mpox cases are surging both in Australia and around the world. An expert reveals how pharmacists can address the rising spread.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => curbing-the-spread-as-mpox-cases-skyrocket
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-18 15:16:33
[post_modified_gmt] => 2024-11-18 04:16:33
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28254
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Curbing the spread as mpox cases skyrocket
[title] => Curbing the spread as mpox cases skyrocket
[href] => https://www.australianpharmacist.com.au/curbing-the-spread-as-mpox-cases-skyrocket/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28257
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28190
[post_author] => 46
[post_date] => 2024-11-18 09:28:17
[post_date_gmt] => 2024-11-17 22:28:17
[post_content] => Constipation can be an embarrassing topic to discuss with your patients. But irregular bowel movements can not only be uncomfortable, but can lead to other health conditions and severely impact a patient’s quality of life.
[caption id="attachment_28205" align="alignright" width="150"] This CPD activity is sponsored by Reckitt. All content is the true, accurate and independent opinion of the speakers and the views expressed are entirely their own.[/caption]
Constipation is a common problem in the community,1 that can significantly impact quality of life if not properly managed.2 It’s also a common reason for primary care visits and referrals to gastroenterologists.3 Unfortunately, many patients are choosing laxatives without the help and advice of a health professional1 so may be choosing products that don’t work effectively5 or choosing to use laxatives when addressing dietary, lifestyle or medicine regimens may be the most appropriate course of action. In this CPD accredited podcast, listen to Priceline Health Services Manager Brett Macfarlane and Senior Clinical Pharmacist – Gastroenterology at the Royal Melbourne Hospital Stephanie Dimovski discuss the problem of constipation and how pharmacists can assist patients in managing this condition. They will address the importance of identifying whether insufficient fibre and fluid intake may be contributing and whether making dietary and exercise recommendations is enough to restore normal bowel habits.
This CPD activity is sponsored by Reckitt. All content is the true, accurate and independent opinion of the speakers and the views expressed are entirely their own.[/caption]
Constipation is a common problem in the community,1 that can significantly impact quality of life if not properly managed.2 It’s also a common reason for primary care visits and referrals to gastroenterologists.3 Unfortunately, many patients are choosing laxatives without the help and advice of a health professional1 so may be choosing products that don’t work effectively5 or choosing to use laxatives when addressing dietary, lifestyle or medicine regimens may be the most appropriate course of action. In this CPD accredited podcast, listen to Priceline Health Services Manager Brett Macfarlane and Senior Clinical Pharmacist – Gastroenterology at the Royal Melbourne Hospital Stephanie Dimovski discuss the problem of constipation and how pharmacists can assist patients in managing this condition. They will address the importance of identifying whether insufficient fibre and fluid intake may be contributing and whether making dietary and exercise recommendations is enough to restore normal bowel habits.
After reading this article, pharmacists should be able to:
|
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 28164
[post_author] => 3410
[post_date] => 2024-11-13 12:50:58
[post_date_gmt] => 2024-11-13 01:50:58
[post_content] => The Therapeutic Goods Administration (TGA) has worked with Phenergan manufacturer Sanofi to develop a new contraindication for the medicine in children under 6.
The decision to restrict use of the medicine in this age cohort – commonly used to treat allergies, travel sickness and nausea – is based on a thorough evaluation of new scientific evidence that the risks outweigh the benefits, a spokesperson for Sanofi told Australian Pharmacist.
‘Following recent evaluations made by Sanofi Consumer Healthcare Pty Ltd, including a benefit-risk assessment, the research has shown a causal association between promethazine and safety concerns,’ said this spokesperson.
The sponsor-initiated update was prompted by advice from the TGA Advisory Committee on Medicines (ACM) – first-generation oral sedating antihistamines – do not use in children, said a spokesperson from the TGA.
‘Further review by the sponsor of cumulative safety data in children 2 to 5 years of age demonstrated sufficient evidence of a causal association between promethazine and psychiatric and central nervous system adverse events in this age group,’ the TGA spokesperson told AP.
The contraindication comes after Medsafe, the New Zealand Medicines and Medical Devices Safety Authority, moved to contraindicate the use of the medicine in children under 6 due to the potential for fatal respiratory depression, psychiatric and central nervous system (CNS) events.
AP understands that the contraindication will affect other products. A spokesperson for AFT said a variation has been submitted to update the product information and label on Allersoothe Elixir with a change to the age indication from children 2 years and older to children 6 years and older. This submission is pending approval.
Will the packaging change?
Not immediately.
New labels for promethazine-containing products will be rolled out in 2025 due to production and logistics lead times, said the Sanofi spokesperson.
‘No immediate action is required regarding current stock. There is no need to set aside existing medications, as this communication does not constitute a recall,’ said the spokesperson. ‘Similarly, the revised labels do not create any changes in the ordering process.
The product information for Phenergan has been updated and is available here.
What should pharmacists do if they get a Phenergan script for an 18 month old infant?
The use of promethazine in children under 6 years of age is now both contraindicated and off label, said Peter Guthrey MPS, PSA Senior Pharmacist – strategic policy.
‘This means that if you choose to dispense, both the prescriber and dispenser carry the full indemnity risk, and you need to get the patient to provide informed consent,’ he said.
Should a parent present with a script for promethazine for use in a child under 6 years of age, pharmacists should contact the prescriber to discuss the risks and benefits, noting that it's contraindicated.
Is there any situation where it would be appropriate to dispense Phenergan to a young child?
It would need to be a pretty compelling case, where the benefit to a child outweighed the risk of respiratory depression, psychiatric or CNS events, said Mr Guthrey.
‘Given it’s a documented contraindication, it'd be pretty hard to demonstrate the medicine is ‘‘safe and therapeutically appropriate’’,’ he said.
‘It is going to be difficult to find a situation where supply is clinically justified and pharmacists have met their obligations to patient safety.’
What about prescribing Phenergan as a Schedule 3 medicine?
If a parent requests promethazine as a Schedule 3 medicine for someone under the age of 6 years, generally alternate products or advice for treatment should be provided following a discussion.
‘While a pharmacist prescribing promethazine as a Pharmacist Only Medicine is lawful for children aged 2-5 years, it is still contraindicated,’ said Mr Guthrey. ‘There would be very few, if any, situations where prescribing the medicine where contraindicated would be warranted.’
What about phenylephrine?
There are some combination phenylephrine products indicated for children under 6 years of age for nasal congestion. However, there is plenty of evidence showing that oral phenylephrine products are ineffective as a nasal decongestant.
In fact, the United States Food and Drug Administration (FDA) recently announced it will move to ban oral phenylephrine products because they simply don't work.
‘Based on our review of available data, and consistent with the advice of the advisory committee, we are taking this next step in the process to propose removing oral phenylephrine because it is not effective as a nasal decongestant,’ said Patrizia Cavazzoni, M.D., director of the FDA’s Center for Drug Evaluation and Research.
While a spokesperson for the TGA told Australian Pharmacist back in July that there are ‘no plans’ to review the effectiveness of oral phenylephrine, it will continue to monitor the outcomes of the FDA review.
What advice should pharmacists provide?
For children with allergies, non-sedating antihistamines are first line.
The best thing parents can do when a child under 6 years of age has cough or cold symptoms is to wait it out, with a review by a medical practitioner when appropriate.
‘It's about reassurance to parents that the cough in itself isn't harmful, and that kids don’t always need medicines for a cold – they need time and supportive therapy,’ said Mr Guthrey.
It’s important that pharmacists give parents confidence that they're doing the right thing by not treating the cough, and providing symptomatic relief for fever and chills – ensuring they are appropriately counselled on when review by a medical practitioner may be appropriate.
For more information, refer to the Australian Pharmaceutical Formulary and Handbook treatment guidelines on:
[post_title] => Do not supply Phenergan to children under 6, manufacturer warns
[post_excerpt] => The TGA has worked with Phenergan manufacturer Sanofi to develop a new contraindication for the medicine in children under 6.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => do-not-supply-phenergan-to-children-under-6-manufacturer-warns
[to_ping] =>
[pinged] =>
[post_modified] => 2024-11-21 09:54:51
[post_modified_gmt] => 2024-11-20 22:54:51
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=28164
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Do not supply Phenergan to children under 6, manufacturer warns
[title] => Do not supply Phenergan to children under 6, manufacturer warns
[href] => https://www.australianpharmacist.com.au/do-not-supply-phenergan-to-children-under-6-manufacturer-warns/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 28167
[authorType] =>
)
Get your weekly dose of the news and research you need to help advance your practice.
Protected by Google reCAPTCHA v3.

Australian Pharmacist is the official journal for Pharmaceutical Society of Australia Ltd.