Young children, elderly patients, Aboriginal and Torres Strait Islander people and pregnant women are susceptible to severe symptoms from various diseases. Despite this risk, vaccination coverage is lower among these groups.
Pharmacists have the opportunity to increase vaccination rates through knowledge of policy, participation in various programs and adopting specific approaches.
1. Low influenza 2023 vaccination rates among young children
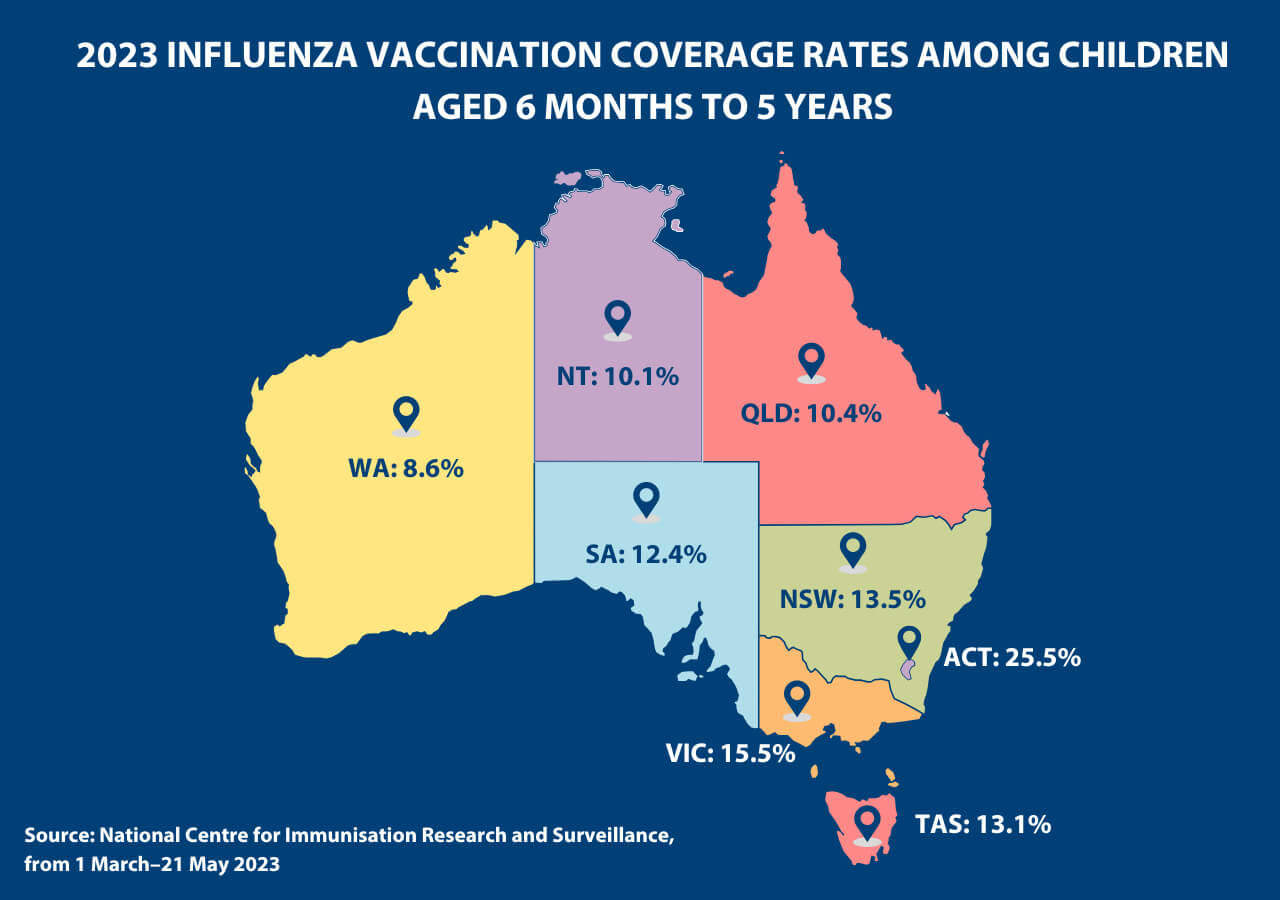
Many of Australia’s youngest patients are not vaccinated against influenza, despite their susceptibility to severe infection, hospitalisation and death. Data from the National Centre for Immunisation Research and Surveillance revealed that in 2023:
- only 12.9% of Australian children aged 6 months to 5 years have been vaccinated against influenza in 2023
- Queensland and the Northern Territory have the lowest vaccine coverage for this age group at 10.4% and 10.1% respectively (from 1 March– 21 May 2023).
 To improve vaccination rates in Queensland-based children, the age regulation for pharmacy vaccination shifted significantly on 1 March 2023.
To improve vaccination rates in Queensland-based children, the age regulation for pharmacy vaccination shifted significantly on 1 March 2023.
‘The fact that Queensland pharmacists have been authorised to vaccinate people [aged 6 months to] 5 years of age against influenza is an absolute game changer,’ said PSA Queensland State Manager Nicole Floyd.
‘As a mother of a 3 year old and 5 year old, this is the first year I have been able to take my entire family to get their influenza vaccination at my local community pharmacy at a time convenient for us.
‘We as a profession have a fantastic opportunity to make a real difference in this cohort and I encourage pharmacists to ensure their local families know they can now immunise the entire family.’
2. COVID-19 vaccinations stall in aged care facilities
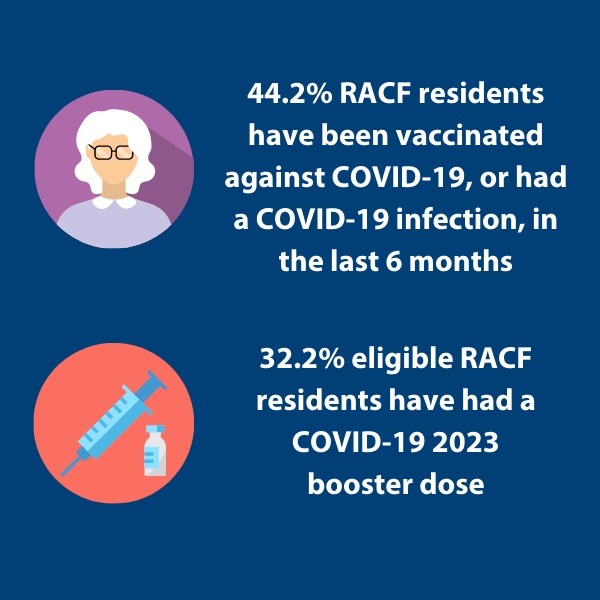
Patients aged 70 years and over are of the most at-risk groups for serious illness from COVID-19. Yet data on the COVID-19 vaccine rollout found that:
- Less than half (44.2%) of all residential aged care facility (RACF) residents have been vaccinated against COVID-19, or had COVID-19 infection (which removes eligibility for vaccination), in the last 6 months.
- Less than a third of eligible residents have had a COVID-19 2023 booster dose.
According to Deputy Chief Medical Officer Dr Michael Kidd, co-administering COVID-19 and influenza vaccinations could increase uptake in eligible patients.
 ‘Of course, as we all know, you can give both on the same day, separate arms, without causing any problems,’ he said.
‘Of course, as we all know, you can give both on the same day, separate arms, without causing any problems,’ he said.
There are also several programs pharmacists can participate in to up vaccination rates, said PSA NSW State manager Amanda Fairjones.
‘Pharmacists are encouraged to engage with their local RACFs to support the administration of 2023 COVID-19 boosters for both residents and any eligible staff,’ she said.
Outreach programs are funded through the Pharmacy Program Administrator, with incentive payments for site visits increasing from 1 February 2023 to $118.15.
Some Primary Health Networks also offer programs to compensate pharmacists and GPs for administering COVID-19 vaccines in RACFs.
‘Through the Southwestern Sydney PHN pharmacies will receive a $250 grant for the first patient or resident they visit, and $150 for each additional resident or patient at the same location,’ said Ms Fairjones.
3. Pregnant women are undervaccinated against influenza and pertussis
From 2012–2017, only about 12% of pregnant Australian women received both the influenza and diphtheria, tetanus and pertussis (dTpa) vaccines across Queensland, Western Australia, and the Northern Territory. These areas collectively represent about a third of all Australian births.
Uptake could be low in this ‘highly anxious group’, as pregnant women are often unwilling to put their unborn child at risk, said Anna Barwick MPS, who provides advice for young mothers through her online Gestational Diabetes Thrive service.

However, pharmacists have a role in educating women about what vaccines to receive and when, along with the benefits to their unborn child, by informing women that:
- the dTpa vaccine is usually administered at 28 weeks pregnancy, however it can be given anytime between 20-32 weeks
- when a dTpa vaccine is administered at least 7 days before birth, 9 out of 10 infants aged <3 months receive protection against hospitalised pertussis
- an influenza vaccine administered during pregnancy protects children against the virus in the first 6 months of life. Pharmacists can administer the vaccine and should offer this early in pregnancy
- both vaccinations are covered under the NIP.
‘Pharmacists are often the first ones to find out that women are pregnant, particularly when they’re after medicines for other conditions, and we’ll often provide them with pregnancy tests,’ said Ms Barwick.
‘So it’s just about reassuring women, not adding to their stress and correcting any misconceptions they might have heard in the media, or from family and friends.’
4. Lower HPV course completion in Aboriginal and Torres Strait Islander patients
There is a disparity between Aboriginal and Torres Strait Islander and non-Indigenous youth in relation to Human Papillomavirus vaccination rates, which could be contributing to an increased incidence of cancer.
Research from the Australian Research of Health and Welfare, the British Medical Journal and the Department of Health and Aged Care has revealed that:
- among young people turning 15 in 2020, 80.5% of girls and 77.6% of boys were fully immunised against HPV, with Aboriginal and Torres Strait Islander coverage rates lower at 75% of girls and 68% of boys
- HPV course completion rates are lower among Aboriginal and Torres Strait Islander adolescents
- throat cancers caused by HPV are 15 times higher in young Aboriginal and Torres Strait Islander patients.
To emphasise the importance of vaccination, Cairns-based embedded Aboriginal Community Controlled Health Organisation pharmacist Kate Gill MPS said pharmacists should ‘go back to basics’.

‘I explain how vaccines work in a very simple way, including likening antibodies to soldiers and drawing pictures, because I’ve found that in some parts of the population up here, there’s a little bit of mistrust,’ she said.
To ensure young Aboriginal and Torres Strait Islander patients receive their full course of HPV vaccination, Ms Gill recommends initiating a discussion about building antibodies.
‘There’s a lack of understanding why they keep needing these injections,’ she said. ‘So you can explain, “the soldiers [are retreating], so you’ve got to bring more into the front line”.’



 Jess Hadley, community pharmacist and Professional Officer at PDL[/caption]
Jess Hadley, community pharmacist and Professional Officer at PDL[/caption]
 Peter Guthrey, Senior Pharmacist – Strategic Policy at PSA[/caption]
Peter Guthrey, Senior Pharmacist – Strategic Policy at PSA[/caption]


 Professor Margie Danchin[/caption]
Professor Margie Danchin[/caption]

 Dr Peter Tenni[/caption]
Dr Peter Tenni[/caption]
 How should we deprescribe gabapentinoids, according to the Maudsley Deprescribing Guidelines[/caption]
How should we deprescribe gabapentinoids, according to the Maudsley Deprescribing Guidelines[/caption]






