With a plunge in vaccination rates following the COVID-19 pandemic peak, a new report says a concerted push is required, with a focus on national consistency.
The Grattan Institute’s A fair shot: How to close the vaccination gap report recommends action on a National Vaccines Partnership Agreement and harmonisation of the state-based regulations that determine pharmacists’ authority to deliver certain vaccines – which currently differ in each jurisdiction.
These recommendations echo PSA’s ongoing calls for a nationally consistent approach to vaccination, and demonstrate just how far we need to go to ensure equitable access to vaccination for all Australians, said PSA National President Dr Fei Sim FPS.
Australian Pharmacist takes a look at the groups with plummeting vaccination rates, and how empowering primary care professionals such as pharmacists can help to lift them.
Older Australians and Aboriginal and Torres Strait Islander peoples are missing out
Recommended vaccine uptake rates have continued to fall over the last couple of years, particularly among vulnerable groups. At the beginning of the 2023 winter, 2.5 million Australians over 65 years of age were not up to date with their COVID-19 vaccinations – a five-fold increase from 2022.
Other findings about COVID-19 vaccination include:
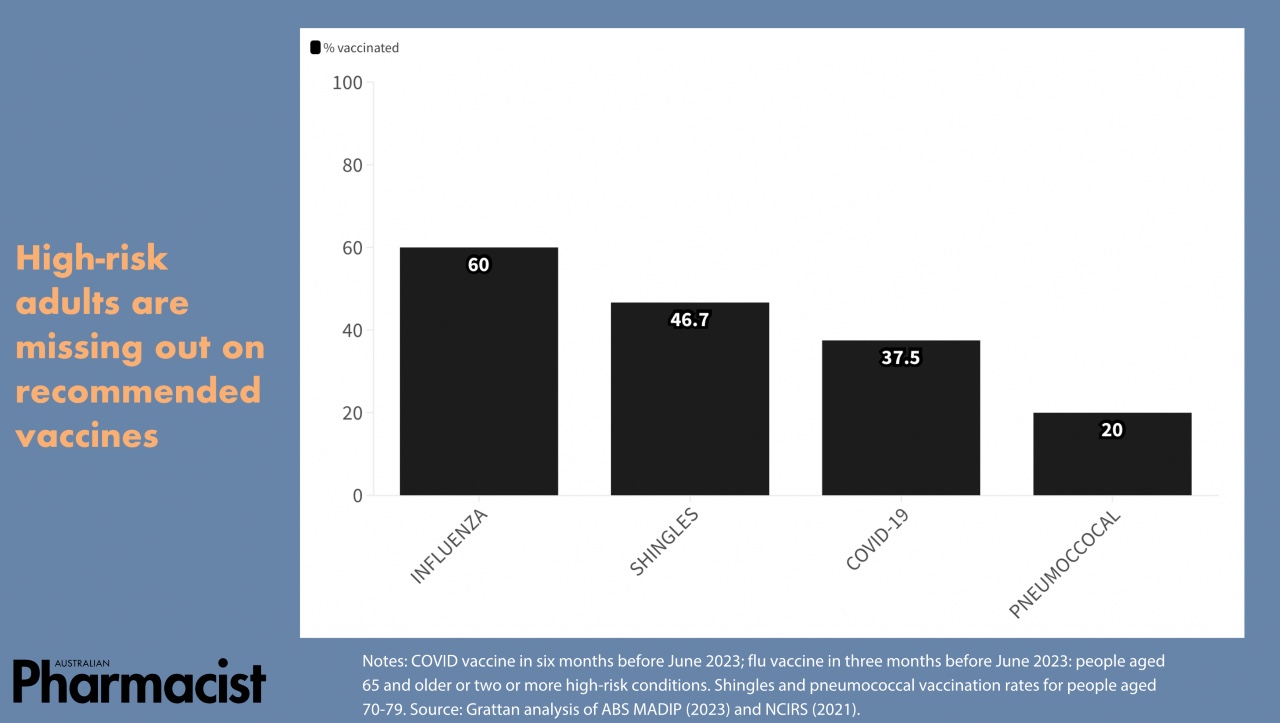
- a crash in up-to-date vaccination from over 90% in December 2021 to less than 10% by the end of February 2023 among those considered high risk
- vaccination rates only reached 38% among high-risk patients following a 2023 COVID-19 booster push
- as of November 2023, less than 4 in 10 aged care residents are considered up-to-date with COVID-19 vaccination.
Older Australians are also behind with other important vaccinations. Less than half of people aged in their 70s were vaccinated for shingles, with even less (one in five) vaccinated against pneumococcal disease.
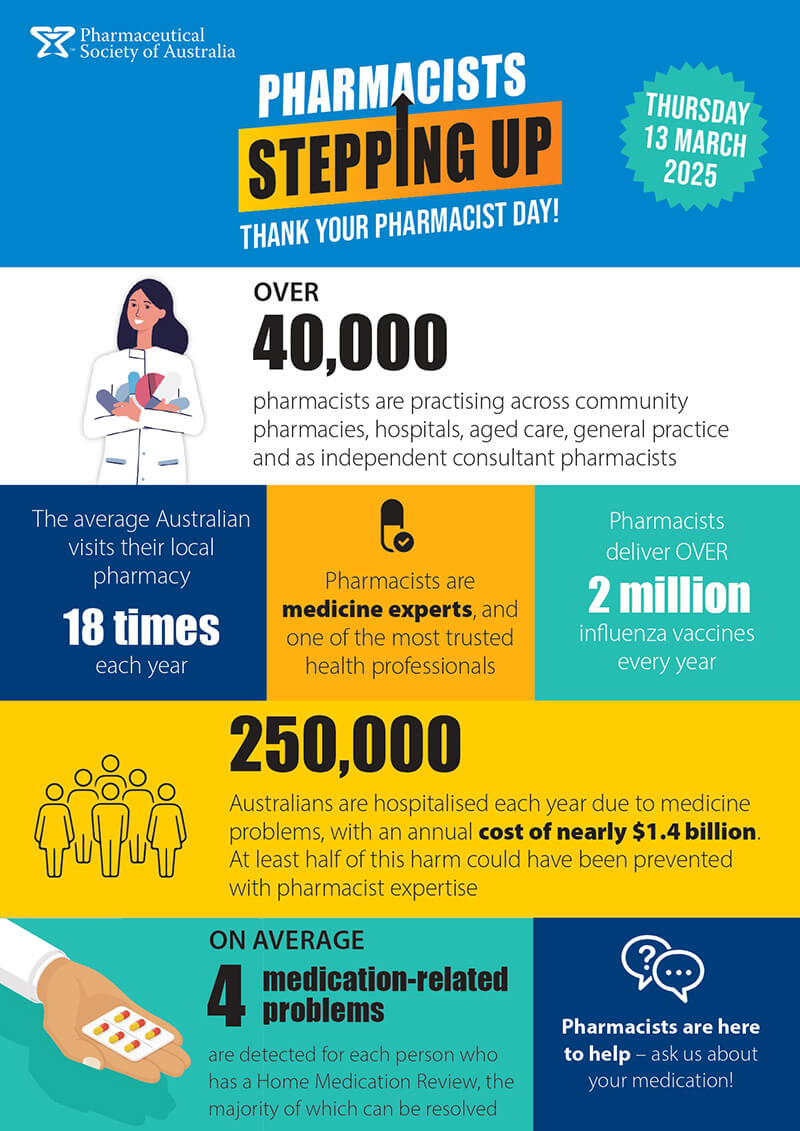
Influenza vaccination rates are also consistently low across the board, with only 27% of Australians vaccinated against influenza in autumn 2023. High-risk groups that receive no-cost vaccinations under the National Immunisation Program (NIP) are beset by low or inconsistent flu vaccination rates, said the report. For example, only around 16% of Aboriginal and Torres Strait Islander people received an influenza vaccination ahead of winter.
The report predicts vaccination rates will fall further due to several factors, including:
- vaccine fatigue
- confusion over which vaccines are needed
- increased vaccine misinformation.
While Australia has very high childhood vaccination rates by global standards, these factors are likely contributing to a decline in vaccination since 2020. Childhood vaccination rates had climbed up to 95%, but the nation is falling back from this highpoint – which is needed to provide adequate protections against many vaccine preventable diseases.
Non-English speakers half as likely to get vaccinated against COVID-19
There are several demographic factors leading to disparities in vaccination rates. Among high-risk adults, vaccination depends on:
- areas lived
- language spoken at home
- level of earnings.
While vaccination rates among Australians should be higher, the report emphasised that they need to be fairer. For example, patients who speak languages other than English at home are reportedly about half as likely to get recommended COVID-19 vaccinations. Those in rural areas are less likely to get vaccinated, with disparities also existing in major cities. For example, there is a nearly 30% variation in flu vaccination rates in different parts of Brisbane.
Empowering pharmacists through red tape removal
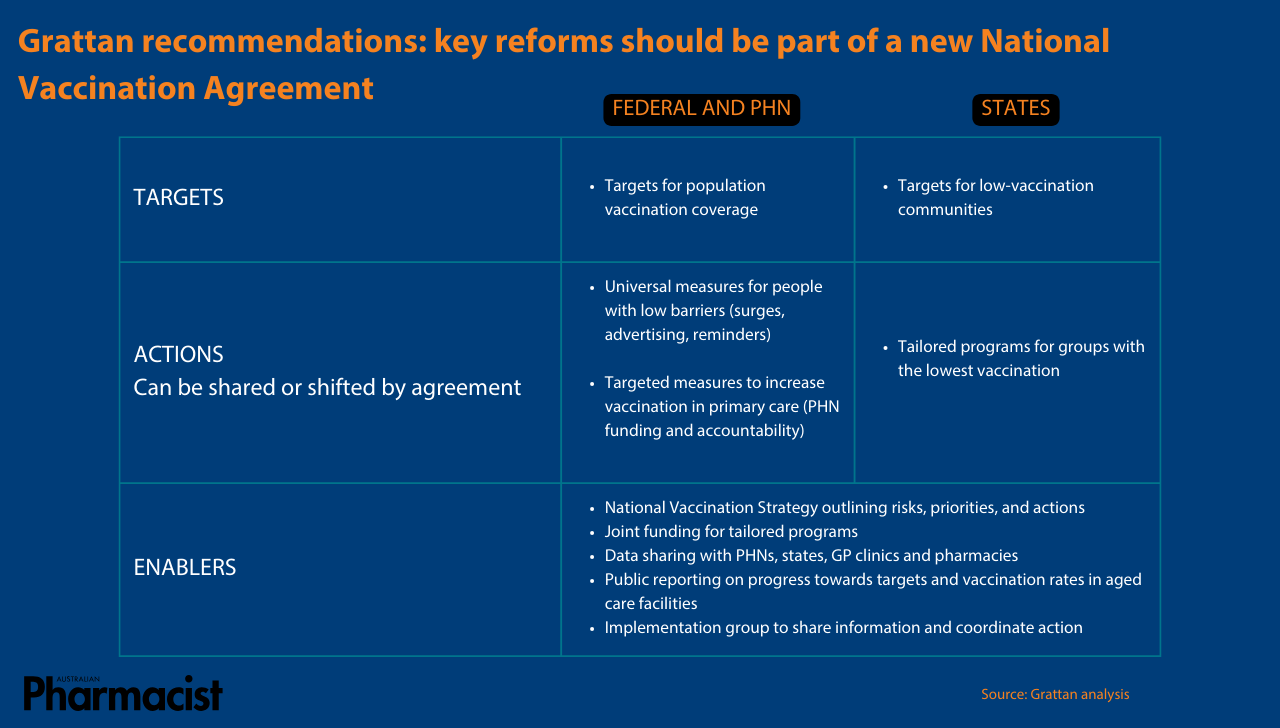
The report calls for a policy reset through a National Vaccination Agreement that outlines clearer goals and responsibilities to boost vaccination targets in high-risk groups.
The report also says that Primary Health Networks (PHNs) should be required to make ongoing progress towards reaching national targets, and must be equipped with funding to support general practice, pharmacists, and aged care providers to promote vaccination in mainstream primary care.
The recent federal government commitment of 4 years of funding to support pharmacists to deliver free NIP vaccines to eligible people will improve access, increasing vaccination locations by up to 60%.
This move will also help to ensure patients can access vaccines from a trusted provider with whom they have an existing relationship.
Crucially, the report argues that ‘the federal government should work with state governments to make pharmacy vaccination regulations consistent across Australia’.
‘State regulations determine whether pharmacists can deliver particular vaccines, who can get particular vaccines from pharmacists, and whether a pharmacist vaccination is free,’ said the report. ‘The federal government’s independent Scope of Practice Review should harmonise these regulations by removing state-specific restrictions, [and] investigate opportunities to remove restrictions on the scope of practice of Aboriginal Health Workers and Aboriginal Health Practitioners.’
A nationally consistent schedule of pharmacist-administered vaccines is key to achieve equitable access to government-funded vaccines by all Australians, agreed Dr Sim.
‘We know that there is no one-size-fits-all approach to improving vaccine uptake, with the report rightly highlighting the need for a tailored approach to ensuring vulnerable cohorts don’t fall through the cracks,’ Dr Sim said.
‘The federal government’s move to open up NIP funding for pharmacist-administered vaccines is a welcome first step, but there is more work to be done to allow pharmacists to deliver all vaccines to patients of all ages.
‘Pharmacists can and should be utilised as trusted health care professionals, working hand in glove with the rest of the primary care team to break down the barriers to vaccination, from improving equity and access, to amplifying public health messages.’







 This article was sponsored and developed in collaboration with PSA and Carers NSW[/caption]
However, pharmacists may perceive medication errors or non-adherence as a carer’s inability to fulfil this role,
This article was sponsored and developed in collaboration with PSA and Carers NSW[/caption]
However, pharmacists may perceive medication errors or non-adherence as a carer’s inability to fulfil this role,